This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
5 Dangers of Birth Control Pills, Plus Side Effects & Alternatives
March 8, 2018

In industrialized nations today, synthetic hormonal oral contraception (aka the birth control pill) is the most common practice for preventing pregnancy. Despite evidence suggesting that there are many possible dangers of birth control pills, millions of women choose to take these hormonal medications every year. In fact, 67 percent of all women who report “practicing contraception” currently use non-permanent birth control methods, primarily hormonal methods — which include the pill, patch, implant, injectables and vaginal ring — or IUDs and condoms. (1) About 25 percent of these women rely on taking daily birth control pills, even though most are aware “the pill” affects their entire bodies.
While birth control pills are convenient and indeed effective at preventing unwanted pregnancies — studies claim they work more than 99 percent of the time when taken correctly, and less than one out of 100 women will get pregnant each year if they always take the pill each day as directed — many feel that as far as their mental and physical health go, the risks of birth control outweigh the benefits. (2)
It’s been found that dangers of birth control pills can include side effects like cystic acne, anxiety or moodiness, breast tenderness, weight gain, or for some difficulty getting pregnant after stopping the pill. Birth control pills may even cause depression.
If you currently use birth control of any kind (the pill, shots, the patch, etc.), I cannot urge you strongly enough to consider natural birth control alternatives instead. There are many other safer ways to prevent pregnancy, such as using condoms or avoiding sex during certain days of the month, that do not cause the side effects associated with taking birth control pills.
What Is a Birth Control Pill?
The Department of Health and Human Services defines birth control pills, also known as oral contraceptives or just “the pill,” as types of medications taken daily by women in order to prevent unwanted pregnancies. (3) While the majority of women choose to take birth control pills so they don’t risk becoming pregnant accidentally, a small percentage also take them for other reasons, including to regulate or temporarily stop their menstrual cycles or reduce symptoms associated with PMS and/or hormonal imbalances (such as acne, heavy bleeding during menstruation or painful cramps).
As of 2012, in the United States alone around 11 million women report using birth control pills, and the number is more than 100 million women worldwide! The total number of women exposed to any type of “synthetic hormonal contraception” is even higher, since most figures don’t account for women using the “morning-after pill” — a type of high-dose hormonal birth control available in the United States without a prescription since 2000. Surveys show that women most likely to take the pill are white women, women in their teens and 20s, never married and cohabiting women, childless women, and college graduates.
Types
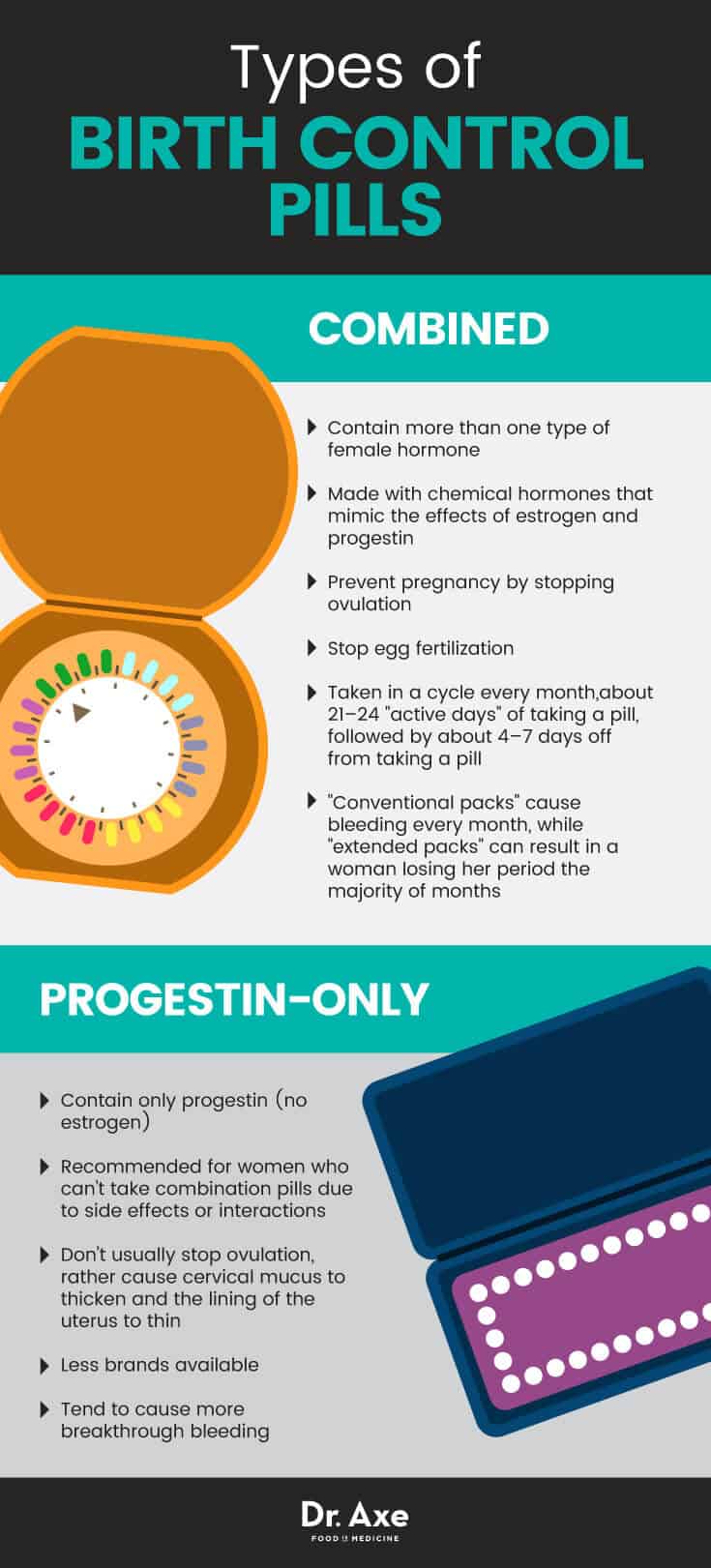
There are dozens of different brands of birth control pills, with most falling into one of two categories: combined pills or progestin-only pills.
Combined birth control pills:
- As the name implies, combine pill birth control medications contain more than one type of female hormone. They’re made with chemical hormones that mimic the effects of estrogen and progestin, which prevent pregnancy by stopping ovulation. Ovulation occurs when the ovaries release an egg every month, which can then lead to pregnancy when the egg is fertilized by sperm.
- In addition to preventing ovulation, combine pill formulas cause other changes to a woman’s reproductive system that stops egg fertilization, including thinning the lining of the uterus and thickening cervical mucus.
- Combined pills are taken in a cycle every month, with usually about 21–24 “active days” of taking a pill, followed by about four to seven days off from taking a pill. Menstrual bleeding usually occurs on the days when pills are taken. Even on days when no pill is taken, the woman still won’t become pregnant.
- “Conventional packs” of birth control pills cause bleeding every month, while “extended packs” can result in a woman losing her period the majority of months. Extended packs can contain up to 84 active pills, which means a woman only bleeds about four times per year (or sometimes not at all). (4)
- Combination birth control pills that contain less than 50 micrograms of ethinyl estradiol (a kind of estrogen) are considered “low-dose pills,” which are usually recommended with women who are sensitive to higher dose brands of birth controls.
Progestin-only birth control pills (sometimes called “minipills”):
- These pills contain only progestin (no estrogen). They’re normally recommended for women who can’t take combination pills due to side effects or interactions.
- Minipills don’t usually stop ovulation, but rather cause cervical mucus to thicken and the lining of the uterus to thin.
- There are far less brands of progestin-only pills available, and they tend to cause more breakthrough bleeding.
Side Effects
Birth control pills, patches and shots promote continuously raised estrogen levels in a woman’s body, something that’s neither natural nor very safe. A woman’s natural menstrual cycle is composed of rising and falling levels of estrogen and progesterone throughout the month. Birth control pills work by keeping estrogen at an unnaturally high level all month long — high enough to even fool the body into thinking it’s already pregnant! Since the body perceives high estrogen levels as a sign of pregnancy, it stops ovulating, and therefore when taking the pill another pregnancy cannot occur.
According to the Food and Drug Administration, it’s been found that the effects of continuously raised estrogen levels in the female body due to taking birth control pills may include: (5)
- Potential increased risk of breast cancer
- Potential increased risk of blood clotting, heart attack and stroke. The risk of blood clots is highest for very overweight women taking the pill.
- Headaches or migraines
- Gallbladder or liver problems, including benign tumors
- Increased blood pressure
- Weight gain
- Mood changes, with some women experiencing symptoms of depression or anxiety
- Nausea, cramping, irregular bleeding or spotting between periods
- Breast tenderness
- The pill also does not protect against sexually transmitted infections, including HIV. Therefore if not using another form of protection/contraceptive method, it’s possible to get any type of sexually transmitted disease your partner might have.
Birth control pills contain the very same sorts of synthetic hormones as hormone replacement drugs commonly used by menopausal or post-menopause women. Researchers have now gathered evidence regarding significant problems associated with the effects of synthetic hormones that some suggest women should not take them at all. The same can be said for birth control pills: While some doctors and health authorities report that they’re “safe and effective,” others strongly recommend avoiding them whenever possible.
What about women who may be taking birth control pills primarily to alleviate PMS symptoms like painful cramping or irregular periods? It may surprise you that for many women the pill seems to do very little to address these concerns. In some cases taking birth control pills can even compound the existing hormonal problem and cause worsened symptoms — although, to be fair, every woman reacts differently (including to different brands or doses of the same type of pill).
Some women have intolerable estrogen-induced side effects from taking the pill that get worse when adding more synthetic hormones to the situation. As Dr. Carolyn Dean, M.D., N.D. explains on her website, cramping or painful and irregular periods are often due to a deficiency of progesterone and an excess of estrogen. So estrogen-containing birth control pills — as are the most commonly prescribed pills on the market now — often compound the problem. Here’s one enlightening quote from Dr. Dean’s website:
“The sex hormone cycle regulates 150 bodily systems all of which are suppressed by hormonal contraceptives and all of which are interrelated to all other body systems (including the endocrine, neurologic and immunologic systems). Therefore hormonal contraceptives impact: energy levels, memory and concentration, motor coordination, adrenalin levels and more …”
Dangers of Birth Control Pills
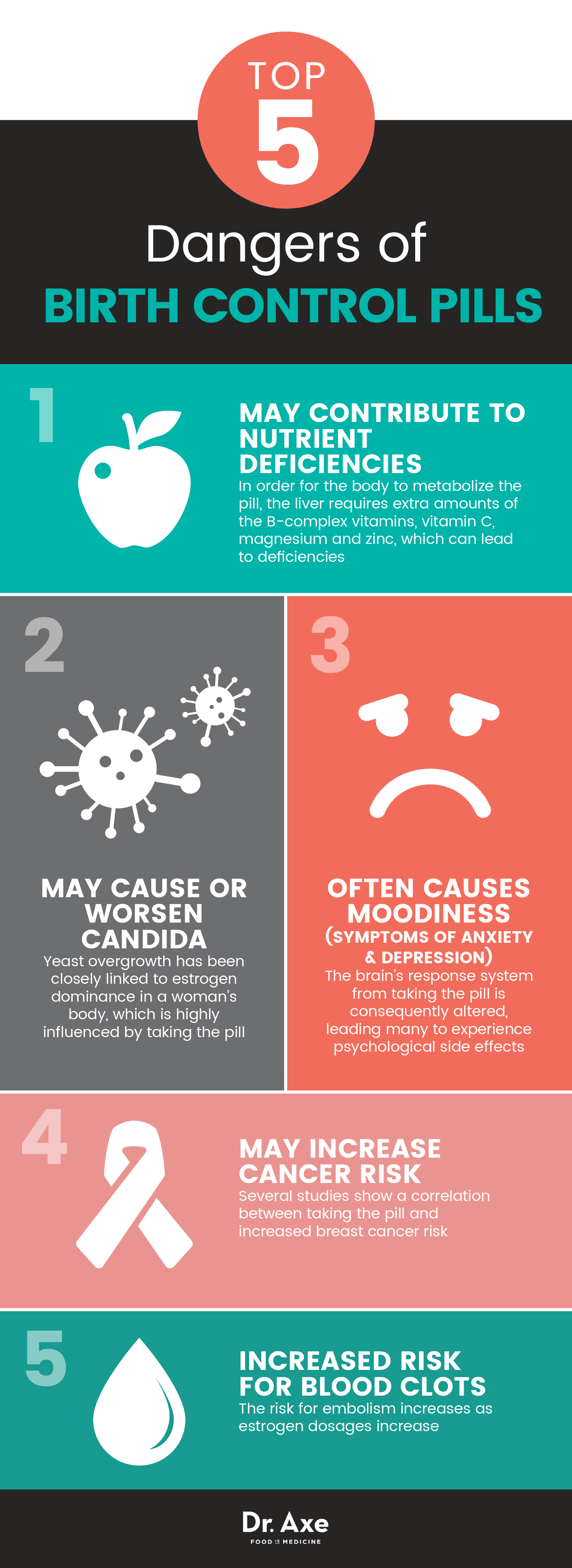
1. May Contribute to Nutrient Deficiencies
Most people don’t know that in order for the body to metabolize the pill, the liver requires extra amounts of the B-complex vitamins, vitamin C, magnesium and zinc. This means that if a woman has been on the pill for years at a time (as many American women are, starting in their 20s or even late teens), she is creating a situation where nutrient deficiency is more likely.
Deficiencies, such as iron deficiency or magnesium deficiency, are some of the primary contributors to most disease (others being factors like diet, genetics, stress and toxicity). If you take the pill, consuming a nutrient-dense, healing diet is key for maintaining gut health and preventing deficiency side effects, like fatigue, indigestion, muscle pains and sleep troubles.
2. May Cause or Worsen Candida
While yeast (candida albicans) generally makes its home in the digestive tract, common lifestyle choices like use of birth control pills, taking antibiotics, a diet high in refined grains and sugar, and high stress levels often lead to a candida overgrowth that infiltrates other parts of the body and leads to candida symptoms.
According to the Healthy Women Organization’s website, yeast overgrowth has been closely linked to estrogen dominance in a woman’s body, which is highly influenced by taking the pill. Women who use hormonal birth control (not just the pill but also a patch or ring) may have more yeast infections than those who don’t. (6)
Toxins from yeast overgrowth can lead to a host of other problems, presenting themselves in a variety of manners far beyond the common vaginal infection. For example, symptoms like migraines, infertility, fibromyalgia, endometriosis, psoriasis, PMS, depression and digestive disorders have all been linked to candida yeast overgrowth. The evidence clearly shows that when you address the yeast overgrowth, the symptoms improve or subside. If you do choose to use birth control pills, try an oral contraceptive that’s a progestin-only pill, since these are linked with occurrence of fewer yeast infections. (7)
3. Often Causes Moodiness (Symptoms of Anxiety and Depression)
Does taking birth control pills cause depression or simply worsen moodiness and existing symptoms? There’s evidence that with estrogen and progesterone levels in the body out of their natural equilibrium due to taking the pill, the brain’s response system is consequently altered, leading many to experience psychological side effects. A proportion of women express concern about low sex drive, lack of appetite, helplessness, disinterest and an overall sad disposition while on birth control pills — yet often their doctors tell them, “It’s all in your head.”
A study conducted in Denmark involving more than 1 million women found a notable increase in depression rates among women taking birth control versus women who were not. Progestin-only pills, the transdermal patch and the vaginal ring were all especially tied to higher ratio of depression diagnoses and antidepressant prescriptions. (8)
To be fair, however, other studies, such as one published in 2012 in the Archives of Gynecology and Obstetrics, have not found the same correlation, so there seems to be individual differences in terms of the pill’s psychological effects. (9) Some evidence now suggests that most of the side effects of hormonal contraception may actually be a result of a psychological stress response to the practice of contraception (wanting to prevent pregnancy despite having sex). (10)
4. May Increase Cancer Risk
The National Cancer Institute tells us that the risk of developing breast cancer is around one in eight for the general public. (11) But studies done by doctors, such as Chris Kahlenborn, M.D., from Altoona Hospital in Altoona, Penn., indicate that “women who took oral birth control before having their first child have a 44-percent increased risk of developing breast cancer.” If this is true, that would bring your risk of developing breast cancer to one in five, a staggeringly high risk.
According to the Breast Cancer Organization’s website: (12)
“There are concerns that because birth control pills use hormones to block pregnancy they may overstimulate breast cells, which can increase the risk of breast cancer. The concern is greater if you’re at high risk for breast cancer because of: a strong family history of the disease, past breast biopsies showing abnormal cells, or you or someone in your family has an abnormal breast cancer gene.”
There is lots of ongoing debate about the breast cancer-depression link. For example, one study published in Cancer Research found a higher risk for breast cancer among women taking high-dose estrogen birth control pills. A review of 54 studies in 1996 found that women have a slightly higher risk of breast cancer while they’re taking birth control pills that contain both estrogen and progestin and during the 10 years after they stop taking the pills. And results from the 2010 Nurses’ Health Study found that use slightly increased risk, especially among women taking triphasic pills, which alter doses of hormones over three stages of the monthly cycle.
Why doesn’t your doctor tell you about this? “There’s tremendous vested interested — drug companies with a lot of money, government agencies who give a lot of money for contraception. It doesn’t make people look good when a study like this comes out,” Dr. Kahlenborn said.
5. Increased Risk for Blood Clots (Pulmonary Problems, Embolism and Thrombosis)
The link between estrogen use and developing blood clots in the veins (called venous thromboembolism) was identified more than 20 years ago. Extensive literature has now been published describing how the risk for embolism increases as estrogen dosages increase. (13) When a clot forms in a deep vein, usually in the leg, it’s called a deep vein thrombosis, and if that clot breaks loose and travels to the lungs, it’s called a pulmonary embolism, which is a serious condition (10 percent to 15 percent of cases cause sudden death). (14) Estrogen seems to increase clotting factors in the blood, making clots more likely.
It’s been found that combination hormonal birth control pills that contain the progestin called desogestrel increase the risk of blood clots more than birth control pills that contain other types of progestin. Birth control pills containing drospirenone are some of the most popular types available and include such brand names as Yaz, Yasmin, Beyaz, Ocella and Zarah. (15)
Shortness of breath, chest pain (particularly with deep breathing), coughing up blood, persistent leg pain, or redness, swelling, or warmth in your lower legs are all signs of clots. The risk is highest among women with family histories of clots, those who smoke and those who are obese/sedentary — so if any of these apply to you, carefully discuss options with your doctor.
Natural Birth Control Alternatives
For centuries, couples have prevented unwanted pregnancies naturally without the use of medications. There are many safe and effective contraceptives to consider that are time-honored strategies, now even being researched and backed up by science. Several birth control options that are natural and don’t require taking medication include:
- Male Condoms: With an approximate 98 percent effectiveness rate when used correctly, they’re nearly as effective as the pill.
- Female Condoms: While these are not as familiar to most people, female condoms are 95 percent effective and are less likely to tear than male condoms. A female condom consists of a small pouch that fits inside the vagina before sex, protecting sperm from entering the female’s body where it can fertilize an egg.
- Diaphragms: These must be fitted by a doctor and are 92 percent to 98 percent effective at preventing pregnancy. They’re thin, soft rubber mounted on rings that are inserted into the upper part of the vagina to cover the cervix and act as a barrier to sperm.
- Cervical Cap: This is a heavy rubber cap that fits tightly over the cervix. It must be put into place by a doctor and can be left in place for 48 hours. These have around a 91 percent effectiveness rate.
- Natural Family Planning/Fertility Awareness: This is an all-natural method for allowing women to track their natural cycles, identify times of fertility, treat premenstrual symptoms and evaluate the effects of stress.
- Calendar Method: Abstention from sex during the week in which a woman is ovulating helps prevent conception from taking place. This technique works best when a woman’s menstrual cycle is very regular and accurately timed. The calendar method doesn’t work very well for couples who use it by itself (about a 75 percent success rate), but it can be effective when combined with the temperature and mucus methods described below.
- Temperature Method: This is a way to pinpoint the day of ovulation so sex can be avoided for a few days before and after. It involves taking the basal body temperature (your temperature upon first waking) each morning with an accurate basal thermometer and noting the rise in temperature that occurs after ovulation. While this method won’t work to prevent pregnancy the first month you start using it, once you have tracked your cycle for several months you can pinpoint which days are the most fertile, and avoid sex on those days. Note that factors like illness or lack of sleep can change body temperature and make this method unreliable by itself, but when it’s combined with the mucus method, it can be an accurate way of assessing fertility. The two methods combined can have a success rate as high as 98 percent.
- Mucus Method: This involves tracking changes in the amount and texture of vaginal discharge, which reflect rising levels of estrogen in the body. For the first few days after your period, there is often no discharge, but there will be a cloudy, tacky mucus as estrogen starts to rise. When the discharge starts to increase in volume and becomes clear and stringy, ovulation is near. A return to the tacky, cloudy mucus or no discharge means that ovulation has passed.
Precautions
The side effects and potential dangers of birth control pills described above apply to some women even more so than others. Factors such as your menstrual cycle history, age, overall health/medical history and use of medications may determine that you should definitely avoid all types of birth control pills (even low-dose options). Your doctor is the best person to help you decide if birth control is a risky or poor option for you.
Women who should be very careful about taking oral contraceptives, due to interactions and side effects, include those who are:
- Already pregnant or breastfeeding. If you’re not sure if you’re pregnant or have unexplained bleeding and irregular periods, be sure to get evaluated before taking any hormonal medications.
- Older than age 35
- Smoke cigarettes or use recreational drugs
- Have a history of high blood pressure, diabetes, stroke, heart disease, current deep vein thrombosis or pulmonary embolism
- Have a history of breast cancer
- Have diabetes-related complications that affect circulation and the nerves (such as diabetic neuropathy, nephropathy or retinopathy)
- Healing from any major surgery
- Take St. John’s wort, anticonvulsant or anti-tuberculous agents that can interact with birth control pills
Final Thoughts
- Birth control pills are used by more than 100 million women worldwide, however there are dangers associated with birth control pills due to unnaturally altering a woman’s estrogen levels, raising them far too high, which often causes symptoms of estrogen dominance.
- Risks associated with birth control pills can include moodiness or depression, breast tenderness, nutrient deficiencies, and possibly a higher risk for certain types of cancers.
- There are safer, more natural means of preventing pregnancy (or addressing the cause of irregular periods and cramping), including using condoms or diaphragms, the temperature method, or the mucus method.







