This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Melasma: Chloasma Causes (+ How to Get Rid of ‘Pregnancy Mask’)
August 26, 2018

Have you ever heard of the mask of pregnancy? It refers to a skin condition that’s triggered by hormonal changes and develops around your forehead, lips, nose and cheekbones. It’s actually common for pregnant women to develop dark, blotchy spots on their face — a condition known as chloasma or melasma. Changing hormone levels stimulate an excess production of melanin, which leads to hyperpigmentation.
Even though chloasma is pretty common among pregnant women, or women taking birth control pills and receiving hormone therapy, it can still be frustrating and embarrassing.
Although the most common form of therapy for chloasma is a combination of topical agents, prolonged use of these agents can lead to side effects like depigmentation and skin irritation. Thankfully, there are some safer alternatives that are out there. Whether it’s focusing on eating nutrient-rich foods that are already part of a healthy pregnancy diet, or using natural skin care remedies, when it comes to improving symptoms of chloasma, you don’t necessarily have to wait until after delivery.
What Is Chloasma?
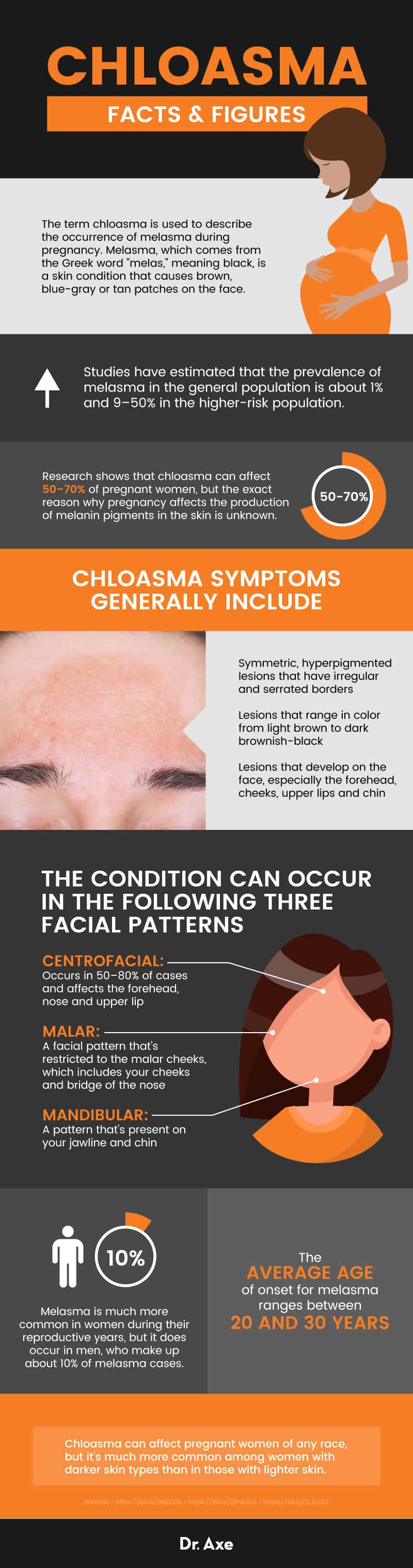
The term chloasma is used to describe the occurrence of melasma during pregnancy. Melasma, which comes from the Greek word “melas,” meaning black, is a skin condition that causes brown, blue-gray or tan patches on the face. Studies have estimated that the prevalence of melasma in the general population is about 1 percent and 9–50 percent in the higher-risk population. (1)
Research shows that chloasma can affect 50–70 percent of pregnant women, but the exact reason why pregnancy affects the production of melanin pigments in the skin is unknown. (2)
In some cases, chloasma lesions disappear within a year after pregnancy or other types of hormonal stimulus, like taking birth control pills. But in persistent types of chloasma, the symptoms are still present one year after the hormonal stimulus is removed and it’s caused by exposure to UV rays.
Signs and Symptoms
Chloasma symptoms generally include:
- Symmetric, hyperpigmented lesions that have irregular and serrated borders
- Lesions that range in color from light brown to dark brownish-black
- Lesions that develop on the face, especially the forehead, cheeks, upper lips and chin
The condition can occur in the following three facial patterns: (3)
- Centrofacial: Occurs in 50–80 percent of cases and affects the forehead, nose and upper lip
- Malar: A facial pattern that’s restricted to the malar cheeks, which includes your cheeks and bridge of the nose
- Mandibular: A pattern that’s present on your jawline and chin
There’s also a newer pattern of melasma that’s called extra-facial melasma, which can develop on non-facial body parts like the neck, sternum, forearms and upper extremities.
Causes and Risk Factors
There are multiple factors that are known to cause melasma, including female hormonal activity. This is why there’s an increased frequency of chloasma occurrence in pregnancy and among women who are taking birth control pills, or undergoing estrogen replacement therapy. It can also occur in men undergoing estrogen treatment for prostate cancer.
Researchers believe that the presence of estrogen receptors on the melanocytes, which are melanin-forming cells in the skin, may stimulate the cells to produce more melanin, causing the dark patches to develop.
One of the most important factors in the cause and development of chloasma is prolonged exposure to ultraviolet rays from sunlight or other sources.
Here are some facts about the risk factors associated with melasma/chloasma: (4)
- Melasma is much more common in women during their reproductive years, but it does occur in men, who make up about 10 percent of melasma cases.
- The average age of onset for melasma ranges between 20 and 30 years.
- Chloasma can affect pregnant women of any race, but it’s much more common among women with darker skin types than in those with lighter skin.
- Having a familial history of chloasma may increase your risk of developing the condition.
- Chloasma is most common in people of Asian and Hispanic origins.
Conventional Treatment
There are many topical medications that are used to treat the various stages of melasma, including the following:
- Hydroquinone: This is the most commonly prescribed topical agent. It’s used to lighten dark patches on the skin. Long-term use of hydroquinone can lead to adverse side effects, including depigmentation (lightening of the skin) and blue-black pigmentation (called exogenous ochronosis).
- Azelaic acid: This is often recommended as an alternative to hydroquinone for the treatment of skin pigmentation.
- Kojic acid: Kojic acid, which is actually made from different types of fungi, is used in cosmetic products as a skin-lightening agent. For some people, it can lead to contact dermatitis and make your skin more susceptible to sunburn.
- Retinoids: Retinoids like tretinoin are commonly used in photoaging therapy and to reverse skin aging. However, some patients experience irritant reactions when using retinoids, including burning, scaling and dermatitis. (5)
- Topical steroids: Topical corticosteroids are commonly used in conventional medicine for a variety of skin conditions because of their anti-inflammatory properties. They are sometimes used in combination with hydroquinone to suppress melanin production. (6)
- Glycolic acid: Glycolic acid is often used in chemical peels or dipigmentation peels. It is a powder made of crystals, so it’s commonly added to cosmetic products as an exfoliating agent.
- Mequinol: Mequinol is often used in combination with a topical retinoid called tretinoin for skin depigmentation. But mequinol should not be used by women who are pregnant because it may cause birth defects.
- Arbutin: Arbutin, which is extracted from the bearberry plant, is used to prevent the formation of melanin and is commonly added to skin-lightening products. However, there’s not enough evidence to fully understand the mechanisms of arbutin for skin care. (7)
Combination therapy is preferred among dermatologists, with the most common combination being hydroquinone, a topical steroid and retinoic acid, according to research published in the Indian Journal of Dermatology. (8)
Aside from topical agents, some other conventional treatments for chloasma include chemical peels, laser therapy or intense pulse light sources. These types of treatments are not considered safe during pregnancy and should be avoided by women with chloasma. (9)
7 Natural Tips to Help Treat Chloasma
The changes to your skin pigmentation during pregnancy will most likely return to normal within a few months after delivery. To safely reduce the darkened spots on your face during pregnancy, there are a few natural remedies that you can try. I recommend running these natural tips to help treat chloasma by your OB-GYN or midwife before starting anything new.
1. Vitamin C Serum
Because of vitamin C, or ascorbic acid’s antioxidant properties, it can be used as a natural remedy for chloasma. It helps to prevent free radical production and the absorption of ultraviolet radiation, according to research published in the Indian Journal of Dermatology. You can use natural skin products containing vitamin C to help brighten your skin or you can make your product, like this DIY Vitamin C Serum for the face.
A double-blind clinical trial has also found that when compared to the treatment of melasma with hydroquinone, ascorbic acid was also effective and was almost devoid of side effects. (8)
A study conducted in the 1980s suggests that a combination of vitamins E and C resulted in significantly better clinical improvement of chloasma than vitamin C alone. But researchers found that when patients were divided into three treatment groups: vitamin C alone, vitamin E alone and a combination of vitamins E and C, all three groups experienced significantly decreased hyperpigmented areas. (10)
2. Consume or Apply Bioflavonoids
Bioflavonoids, or flavonoids, are naturally occurring polyphenolic compounds that have well-known anti-inflammatory and antioxidant properties. They can be beneficial when consumed and even when flavonoid compounds are added to skin care products. This is due to their hypopigmentary effects, which comes from their ability to effect melanin pigmentation. (8)
You can try using a natural formulation that includes flavonoid compounds and increasing your consumption of bioflavonoid-rich foods, such as fresh fruits, vegetables, herbs and spices, teas and high-quality dark chocolate.
3. Apply Apple Cider Vinegar
Apple cider vinegar is known to improve the pigmentation and appearance of skin. It works as a natural toner and can be used to lighten dark patches that are associated with chloasma.
Although there are no studies specifically evaluating the efficacy of apple cider vinegar for melasma, a 2016 randomized controlled trial published in Evidence-Based Complimentary and Alternative Medicine found that using apple cider vinegar topically for the treatment of varicose veins improved symptoms including pigmentation, itchiness and pain. (11)
To use apple cider vinegar for chloasma, you can simply apply a small amount to your skin on a cotton pad after you’ve washed your face with a gentle cleanser. You can also try making my simple Apple Cider Vinegar Toner that’s made with lemon essential oil and witch hazel extract.
Kojic acid is also become a well-known ingredient in topicals used for melasma, as it works to reduce the production of melanin in the skin.
4. Eat Your Lutein
What’s lutein? It’s a type of carotenoid antioxidant that helps to fight free radical damage that’s caused by blue light or sun exposure. Many people know of it as “the eye vitamin,” but it can help with improving chloasma symptoms too.
According to a double-blind, placebo-controlled clinical trial published in Clinical, Cosmetic and Investigational Dermatology, carotenoids like lutein can be used to lighten and improve skin conditions. When 50 healthy participants with mild-to-moderate dry skin were given either a daily supplement containing 10 milligrams of lutein or a placebo daily for 12 weeks, those taking lutein showed significant improvements. Researchers indicated that the lutein supplement improved overall skin tone and has skin-lightening effects. (12)
Although there aren’t any known special precautions for lutein supplements among women who are pregnant and breastfeeding, the safest way to increase your lutein content is to eat high sources of the antioxidant, like kale, collard greens, spinach, broccoli, green beans, eggs and papaya.
5. Rule Out a Zinc Deficiency
A 2018 study published in the Journal of Cosmetic Dermatology evaluated the serum levels of zinc in 118 patients with melasma. Researchers found that there is a significant relationship between low levels of zinc and melasma, as 45.8 percent of patients with the skin condition had a zinc deficiency, compared to 23.7 percent of patients who served as controls. Based on this evidence, researchers indicate that zinc deficiency may be involved in the pathogenesis of melasma. (13)
Zinc is typically included in prenatal vitamins, which you should be taking every day of your pregnancy. You can also increase your levels by eating foods high in zinc, including grass-fed beef, pumpkin seeds, chickpeas, yogurt and spinach.
6. Use Sunscreen and Limit UV Ray Exposure
As part of your treatment plan for chloasma, it’s important that you avoid UV ray exposure, as it can make your symptoms worse. Be sure to avoid direct sun exposure throughout your pregnancy and use a broad-spectrum sunscreen regularly. Research shows that recurrence of chloasma occurs on exposure to sunlight and other sources of ultraviolet rays. (8)
If you do wind up spending too much time in the sun and get a sunburn, soothe the area with a cool compress and apply a natural moisturizer like aloe vera.
When choosing the best sunscreens for your skin, choose from the recommendations made by the Environmental Working Group, which indicates the sunscreens that contain the least amount of damaging chemicals and the most protection against ultraviolet rays. And remember that no sunscreen product is going to last more than two hours max, so thickly apply the sunscreen coating and reapply every time you are out of the water.
7. Lemon Essential Oil
Compounds found in lemon essential oil possess strong antioxidant properties and are capable of inhibiting free radical damage that changes the appearance of your skin. It’s often used in anti-aging management and may help to nourish and tone your skin. (14)
To use lemon essential oil to help improve signs of chloasma, simply place a small amount of your gentle skin cleanser in your hand, add 2–3 drops of lemon oil, combine the two and apply it to problematic areas. You can also combine 2–3 drops of lemon oil with a half teaspoon of coconut oil and apply it directly to your skin. But remember, lemon essential oil can increase your sensitivity to the sun, so completely avoid direct sunlight exposure within 12 hours of using it.
Precautions
In some cases, treatment for chloasma may be put on hold until after delivery. This is because many conventional treatments for chloasma are not deemed safe during pregnancy and because melasma in pregnancy often disappears after the removal of hormonal triggers.
If you plan to use these home remedies for melasma during pregnancy, be sure to speak to your OB-GYN or midwife first. This is always important when you are beginning a new regime during pregnancy.
Final Thoughts
- Melasma is a skin condition that causes brown, blue-gray or tan patches on the face. The term chloasma is used to describe the occurrence of melasma during pregnancy.
- There’s an increased frequency of chloasma occurrence in pregnancy and among women who are taking birth control pills, or undergoing estrogen replacement therapy. It can also occur in men undergoing estrogen treatment for prostate cancer because it is caused by changes in hormonal activity.
- Conventional treatment for melasma is a combination of topical treatments and other options like laser therapy and chemical peels.
7 Natural Ways to Help Treat Chloasma During Pregnancy
- Vitamin C
- Apple cider vinegar
- Lemon essential oil
- Bioflavonoids
- Foods high in lutein
- Ruling out a zinc deficiency
- Protecting your skin from the sun








