This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Endometriosis Symptoms? Learn About Treatments and Diet Changes
April 26, 2023

Endometriosis is one of the most common health issues experienced among women and one of the leading causes of infertility. How common? It’s estimated that over 190 million women worldwide suffer from endometriosis symptoms.
If you suffer pain and discomfort in your reproductive region, endometriosis may be the reason why. The good news is there are endometriosis treatment options to deal with this uncomfortable condition.
Because there are so many treatment options, and each woman responds to medications and supplements differently, it often requires a period of experimentation to treat endometriosis. Education is key — you know your body better than anyone else, so become familiar with the root causes and treatments (both conventional and natural) before opting for a more drastic surgical procedure.
Learn what exactly endometriosis is, why endometriosis symptoms occur and how you can treat them.
What Is Endometriosis?
Endometriosis is a condition in which tissue, similar to the lining of the uterus, grows in other areas of the body. The female reproductive system includes the vagina, uterus, fallopian tubes and ovaries.
During a normal menstrual cycle, the ovaries make hormones, which signal the lining of the uterus to thicken. This is called the endometrium — the inner mucous membrane of the uterus. The endometrium builds up in preparation to receive a fertilized egg. If the egg is never fertilized, this leads to menstruation, or the shedding of the lining.
For people with endometriosis, the lining tissue grows outside of the uterus. The misplaced tissue responds to the hormones by thickening and shedding with every menstrual cycle; however, the thick tissue is outside of the uterus and is unable to pass through the vagina and out of the body. The endometrial flow is then trapped and may cause inflammation and pain. Adhesions, or scar tissue, may form and stick to one organ to another. It can even cause the fallopian tubes to close, which is a dangerous endometriosis symptom because it can lead to infertility.
Another scary endometriosis symptom is the formation of endometrioma — known as dark, reddish-brown cysts or fluid-filled sacks on the ovaries that affect fertility. Endometriosis may also result in abnormal bleeding.
It’s stated in studies that 40 percent to 60 percent of women who have very painful periods also have endometriosis, and 20 percent to 30 percent of women who are unable to get pregnant are believed to have this disease. Being in tune with your body and having a knowledge of common endometriosis symptoms are helpful.
There is currently no cure for endometriosis, but various treatments are used to relieve the symptoms. Some medication options, like hormonal therapy, can increase the risk of long-term infertility and cancer. If endometriosis symptoms become too severe, surgical procedures may even be necessary.
Fortunately, there are natural remedies for endometriosis that can be utilized before turning to hormone treatments or invasive surgical procedures.
Symptoms
Because 2 percent to 50 percent of women are thought to have “silent” endometriosis — displaying only subtle symptoms or no clinical symptoms at all — it’s important to be aware of the endometriosis symptoms. Endometrial tissue, or implants, can grow in the outside of the womb or in the wall of a fallopian tube.
The disease often affects the ovaries, the “Pouch of Douglas” — which is between the womb and the rectum at the end of the bowel — and the connective tissue in this area. It is when the ovaries or fallopian tubes are affected that women experience fertility problems.
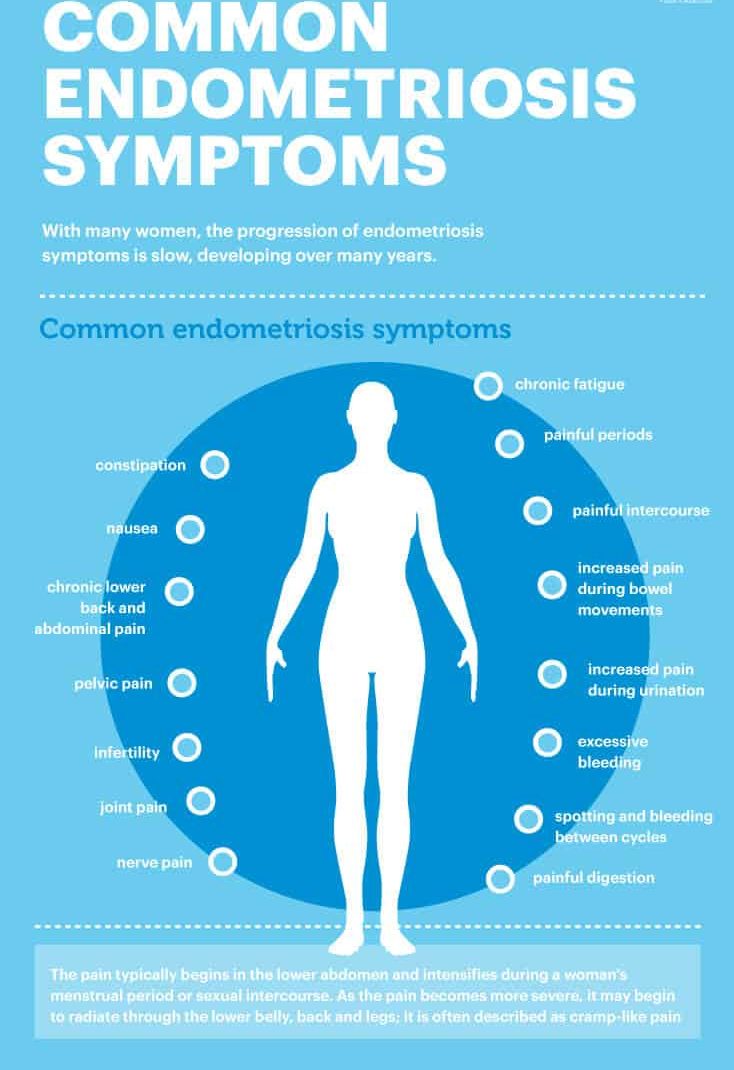
Common endometriosis symptoms include:
- painful periods (also known as dysmenorrhea) or irregular periods
- painful intercourse
- increased pain during bowel movements
- increased pain during urination
- excessive bleeding
- spotting and bleeding between cycles
- painful digestion
- constipation
- nausea
- chronic lower back and abdominal pain
- pelvic pain
- infertility
- joint pain
- nerve pain
- chronic fatigue
- bloating
With many women, the progression of endometriosis symptoms is slow, developing over many years. Each woman experiences a different range of pain, which can make a diagnosis difficult. The pain typically begins in the lower abdomen and intensifies during a women’s menstrual period or sexual intercourse. As the pain becomes more severe, it may begin to radiate through the lower belly, back and legs — it’s often described as cramp-like pain.
Causes
The root cause of endometriosis in unclear, but there appears to be a strong genetic link within families. It’s agreed that endometriosis is not contagious, thus it can’t be transmitted through sexual intercourse.
Endometriosis affects women in their reproductive years. Estimates suggest that 20 percent to 50 percent of women who are treated for infertility have endometriosis. Beginning menstruation early in life, delaying pregnancy until an older age, never giving birth and experiencing menopause later in life may also increase the risk of endometriosis.
There are some other theories pertaining to the causes of endometriosis. One such theory is that menstrual flow is backed up into the fallopian tubes and pelvic and abdominal cavity during menstruation, causing the endometrial tissue to grow outside of the uterus.
Another possibility is coelomic metaplasia — when areas lining the pelvic organs contain primitive cells that can grow into other forms of tissue, such as endometrial cells.
The direct transfer of endometrial tissues during surgical procedures may also serve as an explanation of endometriosis symptoms. The cells may be transferred through the bloodstream or lymphatic system during surgeries, such as a cesarian section or episiotomy. The scar tissue may also contain endometrial cells that will then grow outside of the uterus.
A final explanation is that there is an issue with the interaction between a woman’s hormones or her immune system. Our immune system is supposed to ensure that tissue from a particular organ does not grow elsewhere in the body, so some fingers are pointed at the immune system for allowing endometrial tissue to grow outside of the uterus.
Conventional Treatments
Unfortunately, conventional treatments for endometriosis can require a period of experiments in order to find what works. Pain medication is typically prescribed to treat the pain but not the underlying issue. Hormone treatments, such as hormonal contraception or hormonal therapy, are a common path that doctors pursue. They regulate hormones, slow down the growth of endometrial implants and decrease menstrual flow.
Common conventional treatments include:
Medications
1. Lupron
Lupron is an injection that’s used to induce a hormonal and menstrual suppression in patients with endometriosis, resulting in alleviation of pain symptoms. The most common side effects include decreased blood pressure, redness, pain and burning at the sight of injection, fatigue, headache, upset stomach, and muscle aches.
2. Progestins
Progestin is a drug that behaves like the female hormone progesterone. Progestins work by suppressing the growth of endometrial impacts and reducing endometriosis-induced inflammation in the pelvic cavity.
During the treatment, women lose their periods and ability to conceive. Women who have had long-acting injections may experience prolonged delays in the return of menstruation after treatment.
Like all hormone medications, there are some common side effects, including acne, bloated stomach, bleeding, breast discomfort, depression, fatigue, headaches, upset stomach, nausea, vomiting and weight gain. These side effects can be difficult to live with, and some women cannot complete a course of treatment because they find them intolerable.
3. Danazol
Danazol is a synthetic steroid that serves as a mild androgen (hormones produced by the male testes) but has no estrogenic or progestational properties. Androgens are responsible for the functioning of the male reproductive system and the development of male characteristics, such as facial hair and a deep voice.
Danazol is used to suppress the growth and development of endometrial tissue. The hormonal environment caused by danazol stops menstruation as well. Because it serves as a synthetic male hormone, danzol has androgenic side effects, such as weight gain, increased body hair and acne, decrease in breast size, deepening of the voice, water retention, and oily skin or hair.
Surgical Procedures
1. Laparoscopic Excision or Ablation Surgery
Laparoscopic surgery is the most common procedure utilized by doctors for the treatment of endometriosis. The surgeon makes a small incision to insert a lighted viewing instrument called a laparoscope. This allows the surgeon to view the internal organs in order to look for signs of endometriosis and remove any visible endometriosis implants and scar tissue that can cause pain or infertility. If a cyst is found, that is removed as well.
During the procedure, the patient’s abdomen is inflated with gas, which pushes the abdominal wall away from the organs so the surgeon can see clearly. The scar tissue or implants are removed by cutting them (excision) or destroying them with a laser bream or electric current (ablation). Ablation is typically used on very small lesions, with excision as the preferred technique for large lesions, as it involves less risks.
The risks of laparoscopic surgery include pelvic infection, uncontrolled bleeding, scar tissue formation, and damage to the bowel, bladder or ureters.
2. Hysterectomy
A hysterectomy is the surgical removal of the uterus through the abdominal wall or vagina. A total hysterectomy involves removing the entire uterus, including the body of the uterus and the cervix. A subtotal hysterectomy is the removal of the uterus but not the cervix. Other organs may also be removed during a hysterectomy, including the ovaries and fallopian tubes.
A hysterectomy does not guarantee relief from all endometriosis symptoms because there may still be endometrial tissue left inside the body after the removal of the uterus. According to a 2014 review published in Facts, Views & Vision in ObGyn, a high recurrence rate of 62 percent was reported in advanced stages of endometriosis in which the ovaries were conserved. Based on the 77 articles that were identified for the review, incomplete excision of endometriosis is the most predominant reason in the literature for the recurrence of endometriosis symptoms.
Does Endometriosis Increase the Risk of Cancer?
Research suggests that women with endometriosis have a higher risk of developing ovarian, breast and endometrial cancer. According to a study published in Obstetrics and Gynecology, endometrial cancer has increased 21 percent in incidence since 2008, and the death rate has increased more than 100 percent over the past two decades.
Endometrial, ovarian and breast cancers are associated with several risk factors, such as low parity, infertility, menstruating at an early age and experiencing menopause symptoms at a late age.
A scientific review conducted in Italy investigated the possible role of endometriosis and infertility in increasing the risk of cancer. Many studies showed that women affected by infertility may be more at risk for endometrial cancer, particularly if affected by ovulatory disorders. Furthermore, infertility and endometriosis are now often treated with medical devices that could by themselves modify the hormonal environment of a woman’s body and serve as cofactors in the cellular changes toward cancer development.
The researchers conclude that there are no firm answers about the precise effects of infertility and endometriosis and their treatments on cancer risk, but further studies involving participants undergoing fertility drug treatments and treatments for ovulatory disorders are in order.
Another study published in the American Journal of Obstetrics and Gynecology followed records of 20,686 women hospitalized with endometriosis from 1969–1983 and the National Swedish Cancer Registry through 1989 in order to identify subsequent cancer diagnoses. Fifty-five percent of these women underwent gynecological operations as a result of an endometriosis diagnoses.
After following these subjects for over 11 years, significant excessed cancer risks were observed for breast cancer, ovarian cancer and hematopoietic malignancies. The risk of ovarian cancer was particularly elevated among subjects with a long-standing history of ovarian endometriosis. The researchers suggest that based on the these findings, further attention should be given to the risk of breast, ovarian and hematopoietic cancers among women with endometriosis and exploring possible hormonal and immunologic reasons for excess risks.
Because of this increased risk of cancer that is apparent in several studies, women with endometriosis should be more vigilant. Be sure to get cancer screenings, like mammograms. Pay attention to your body and aware of early signs of ovarian cancer, such as bloating, pelvic or abdominal pain, difficulty eating, and a frequent need to urinate. Discuss the increased risk of cancer with your health care provider, and set up a plan for prevention, such as reducing stress, eating a healthy and anti-inflammatory diet, and engaging in physical exercise.
Natural Ways to Relieve Symptoms
1. Healthy Diet
When attempting to relieve endometriosis symptoms naturally, begin by eliminating foods that lead to inflammation. This includes dairy, processed foods, refined sugars, caffeine and carbohydrates. Eliminate these foods from your diet for at least three weeks, paying close attention to your body changing throughout the process. Alcohol, soy and other high-estrogen foods should also be eliminated from your diet because of their estrogenic effects.
According to a review published in Reproductive Biomedicine Online, women with endometriosis seem to consume few vegetables and omega-3 fatty acids and more red meat, coffee and trans fats. Allergy testing may also be beneficial in order to find out what foods lead to inflammation in the body.
It’s important to follow an anti-inflammatory diet when dealing with endometriosis. A 2004 study published in Human Reproduction found that there is a significant reduction in risk of developing endometriosis in women who consume green vegetables and fresh fruit.
That means it’s a good idea to crowd in these super beneficial anti-inflammatory foods such as green leafy vegetables, celery, beets, blueberries, salmon, bone broth, walnuts, flaxseeds and more.
Magnesium-rich foods also help soothe the uterus and reduce pain. These include pumpkin seeds, sunflower seeds, black beans, avocado, almonds, bananas, chard and spinach. Iron-rich foods are important as well because they replenish the loss of iron in the body, which is a result of excess bleeding. Some foods containing iron include liver, beef steak, navy beans, black beans, spinach, egg yolk, prunes, artichokes and collard greens.
In addition, you can reduce inflammation, relieve joint and muscle pain, and regulate hormone production with omega-3 foods. Add flaxseeds, chia seeds, walnuts, salmon, trout, tuna, sardines, anchovies and mackerel to your diet.
If you are suffering from constipation as an endometriosis symptom, eat high-fiber foods like quinoa, vegetables, brown rice, berries, coconut, figs, artichokes, peas, okra, Brussel spouts, turnips and acorn squash.

2. Supplements
There are certain supplements that can benefit endometriosis sufferers — such as progesterone cream, fish oil, vitex, milk thistle and more.
Pycnogenol is a French maritime pine bark extract that has been used as a natural remedy to treat endometriosis. In a study published in the Journal of Reproductive Medicine, 58 women with endometriosis were followed at four, 12, 24 and 48 weeks after starting treatment to check for endometriosis symptoms. Thirty-two patients in the pycnogenol treatment group took 60 milligrams orally per day for 48 weeks. The 26 other patients were treated in the standard way, using gonadotropin-releasing hormone agonist.
Treatment with pycnogenol slowly but steadily reduced endometriosis symptoms, while treatment with hormone therapy reduced the symptoms more effectively at first, but 24 weeks after the end of treatment, the scores suggested a recurrence of signs. There was no influence on menstrual cycles or estrogen levels with pcynogenol treatment, while menstruation and estrogen levels decreased with hormone therapy. The researchers concluded that pycnogenol serves as a therapeutic alternative to hormone therapy in the treatment of endometriosis.
You can also take 50 milligrams of vitamin B complex daily to balance hormone levels. B vitamins benefit overall health and reduce toxicity in the body, supporting cellular function. They also regulate and balance the body’s organs and support healthy immunity. Vitamin B6, for example, relieves chronic pain, boosts mood and increases energy levels.
3. Acupuncture
A study conducted at Harvard Medical School found that Japanese-style acupuncture may be an effective, safe and well-tolerated adjunct therapy for endometriosis-related pelvic pain.
For the study, 18 young women, ages 12–22 with laparoscopically diagnosed endometriosis-related chronic pelvic pain were analyzed. Participants in the active acupuncture group experienced 62 percent less pain after four weeks, which differed significantly from the control group’s average reduction.
4. Essential Oils
Castor oil can be used to boost immune function and soothe digestion, and castor oil packs can be used on the lower abdomen and pelvic area to reduce pain and inflammation.
In addition, clary sage helps balance hormones naturally and has been found to effectively reduce pain and cramping when applied topically. Apply two to four drops topically over the abdomen, and then apply a warm compress over the area to relieve the pain.
Final Thoughts
Endometriosis symptoms unfortunately occur in a large percentage of women of reproductive age, but there are steps you can take to prevent and treat this disease. The first step is knowing and identifying symptoms so you can find the proper methods of treatment.
If you eat an anti-inflammatory diet and consume beneficial supplements, you can curb endometriosis — as is the case with most conditions. In addition, acupuncture and essentials can do wonder, and by combining these four natural remedies, you can help avoid unnecessary and dangerous surgery.
While there is no cure, if you follow these steps, you can manage, treat and even prevent endometriosis symptoms from becoming a major hindrance on your life.



