This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Relieve Pelvic Pain With 8 Natural Treatments
March 28, 2024

Most people have experienced pelvic pain at some point in their lives. It can be a symptom of constipation or PMS, and it may only occur once in a while. But for some, it is a chronic condition that hinders their ability to do common activities like walking, lifting objects, going to the bathroom or having sex.
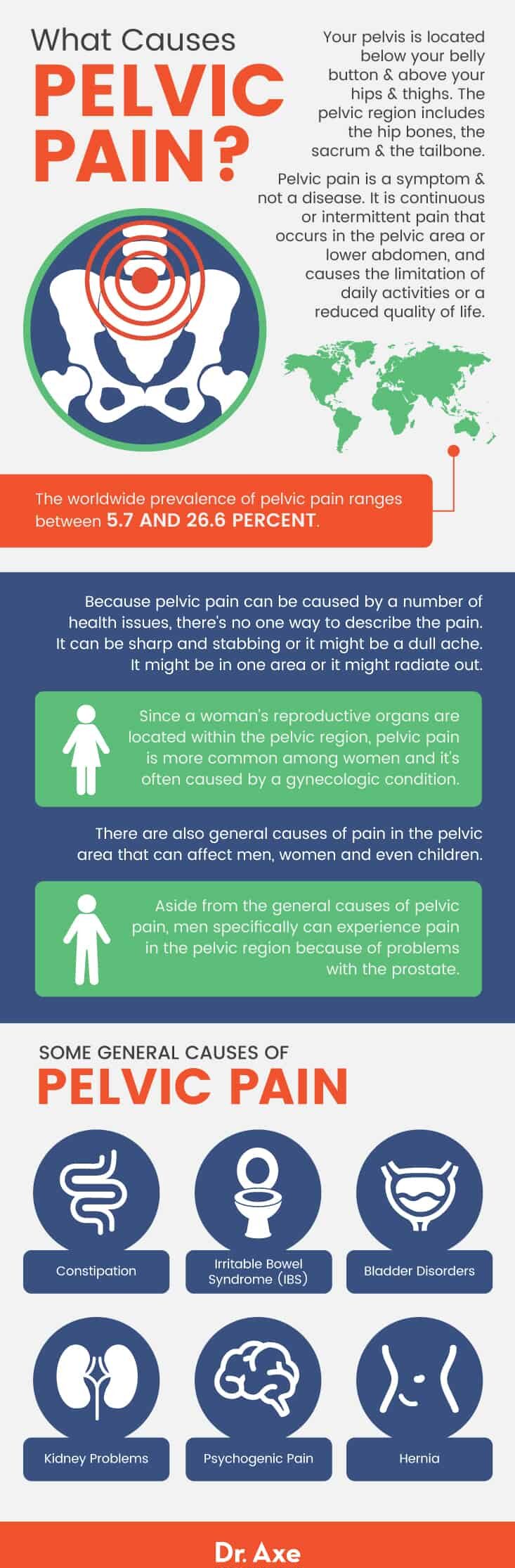
According to research published in Pain Physician, the worldwide prevalence of pelvic pain ranges between 5.7 and 26.6 percent. Although pelvic floor pain is a common complaint among women with gynecologic conditions, it can also be a problem for men who are struggling with digestive, neurological, skeletal, prostate health or inflammatory issues. Pelvic pain can also be a symptom of trauma, chronic stress and mental health issues.
The truth is that two-thirds of patients with chronic pelvic pain have not been given a definitive diagnosis, which can be extremely difficult and frustrating. For many people, the inability to make a clear diagnosis also leads to a lack of progress in the management of this condition. But knowing the possible causes of pelvic pain can help you to distinguish the culprit and get help so that this pain is a concern of the past.
What Is Pelvic Pain?
Your pelvis is located below your belly button and above your hips and thighs. The pelvic region includes the hip bones, the sacrum and the tailbone. People with pelvic pain can experience a shooting, stabbing or aching sensation anywhere within the pelvic region. For some people, the pain begins in another part of the body, like the thighs or lower back. Then spreads to the pelvis.
Because pelvic pain can be caused by a number of health issues, there’s no one way to describe the pain. Because a woman’s reproductive organs are within the pelvic region, pelvic pain is more common among women and it’s often caused by a gynecologic condition. But there are also general causes of pain in the pelvic area that can affect men, women and even children.
Symptoms
Pelvic pain is a symptom and not a disease. It is continuous or intermittent pain that occurs in the pelvic area or lower abdomen, and causes the limitation of daily activities or a reduced quality of life.
The symptoms of pelvic floor pain vary from patient to patient. Some experience intense pain, while others describe it as mild pain. For some men and women, the pelvic pain can be so severe that it interferes with their ability to engage in normal activities, like exercising, working, walking, lifting objects or having sex.
The location of pain can also vary. Pelvic pain can be a sharp, stabbing pain that affects one particular spot in the pelvic area. Or it can be a dull or mild pain that’s spread out or even radiates to the thighs and legs.
Pelvic pain is often associated with other issues, such as urinary symptoms, sexual dysfunction or painful menstrual periods.
Causes & Risk Factors
There are many possible causes of pelvic pain for both men and women. It can be caused by an infection, an issue with non-reproductive internal organs, like the colon or bladder, or for women, a problem with a reproductive organ. Here’s a rundown of the most common causes of pelvic pain:
General Causes
- Constipation: Constipation can cause pain in the pelvis because of the pressure and bloating in your abdomen. There are many factors that lead to constipation, including poor diet, stress, hormonal problems, an imbalance in intestinal flora, a magnesium deficiency and inactivity. Using natural constipation relief remedies can help to reduce pelvic pain in these cases.
- Irritable bowel syndrome: Irritable bowel syndrome is a digestive disorder that can cause cramps, aches and pain in the abdomen and pelvic area. People with IBS symptoms usually find relief after going to the bathroom normally for several days in a row. However, pelvic pain caused by IBS can be recurring. The condition usually involves a cluster of symptoms (like constipation, diarrhea, bloating and gas) occurring together.
- Bladder disorders: When the bladder becomes inflamed, this can create pain in the lower abdomen and pelvic area. One bladder disorder that may be causing such pain is interstitial cystitis, a chronic bladder issue that causes urinary tract infection symptoms. Aside from pelvis pain, people with bladder disorders like interstitial cystitis (also called bladder pain syndrome) may also experience bladder pain that gets worse when the bladder fills, lower back and abdomen pain, frequent urination and a constant urge to urinate.
- Kidney problems: Problems with the kidneys, like a kidney infection or kidney stones, can lead to pelvic pain. Kidney stones, for example, can cause lower back pain that spreads down below the kidneys, to the groin, pelvic area and thighs.
- Hernia: A hernia, which is an abnormal opening or defect that allows organs or tissues to protrude, can cause sharp, shooting and radiating pelvic pain. The location of the pain depends on the location of the hernia. So people with pelvic floor hernias are likely to experience pelvic floor pain. This type of hernia is more common in women because they have a broader pelvic inlet and undergo stresses to the area, such as pregnancy, labor and delivery.
- Psychogenic pain: Research shows that chronic pelvis pain can be associated with a history of sexual trauma. Psychogenic pain refers to the understanding that strong emotions and fears can cause prolonged and even chronic pain. When all causes of pain are ruled out by a health care professional, the pain may be attributed to the patient’s emotional state or past traumatic experiences. In these cases, psychotherapy and counseling can be extremely beneficial.
Causes in Women
Pelvic pain in women can be caused by gynecologic conditions or inflammation. For many women, pelvic pain is the result of a problem with one of the organs in the pelvic area, such as the vagina, cervix, fallopian tubes, ovaries or uterus. It’s also possible to experience pelvic pain as a result of two conditions or problems at the same time. Some of the conditions that can lead to pelvic pain include:
- Endometriosis: Endometriosis is a condition in which the endometrium, the inner lining of the uterus that’s made of mucous membranes, grows outside of the uterus and can’t pass through the vagina during menstruation. When the lining tissue grows and becomes thicker, it can cause endometriosis symptoms like pelvic pain, lower back pain, inflammation, painful periods, bloating and painful digestion.
- Fibroids: Fibroids are non-cancerous tumors that are found within the uterine walls. Research shows that 40 to 80 percent of women in their reproductive years experience fibroids. And one of the most common symptoms of fibroids is pelvic pain or pressure. Other symptoms include bloating or fullness in the pelvic region, pain with intercourse and heavy menstrual bleeding.
- Pelvic inflammatory disease: Pelvic inflammatory disease is an infection of a woman’s reproductive organs that is often caused by some kind of sexually transmitted disease, such as chlamydia or gonorrhea. Common symptoms of pelvic inflammatory disease are pelvic pain, pain or bleeding during sex, a burning sensation when urinating, bleeding between periods, an unusual discharge from the vagina and fever.
- Ovarian cysts: Ovarian cysts are fluid-filled sacs in or on the surface of an ovary. Most ovarian cysts are harmless and don’t cause discomfort. But women with a large ovarian cyst may experience dull or sharp pelvic pain on the side of the body where the cyst is located.
- Ovarian remnant syndrome: Ovarian remnant syndrome occurs when ovarian tissue is left after an oophorectomy, a surgical procedure that involves removing both ovaries and fallopian tubes. The most common symptom of ovarian remnant syndrome is chronic pelvic pain, along with painful urination, bowel movements and intercourse.
- Miscarriage: The most common symptoms of miscarriage are vaginal bleeding and cramps in the lower abdomen, which can feel like pain in the womb. Some women also experience pelvic pain, diarrhea, pain while using the bathroom and feeling faint. Women who are experiencing intense pelvic pain while pregnant should report it to their doctor immediately.
- Menstrual cramps: Some women experience pelvic pain during their period called dysmenorrhea. It can be caused by the muscle contractions in the uterus. Another possible cause of painful cramps and pelvic pain during menstruation is an underlying condition, like fibroids, endometriosis and pelvic inflammatory disease. These conditions alter hormone levels, cause inflammation and put pressure on the uterus. It’s also possible to experience pelvic pain as part of your PMS symptoms, which can be caused or intensified by hormonal imbalances, stress, anxiety or depression, obesity and lack of exercise.
Causes in Men
Aside from the general causes of pelvic pain, men specifically can experience pain in the pelvic region because of problems with the prostate. The following is one of the most common causes of pelvic pain in men:
- Prostatitis: Causes of pelvic pain that are sometimes found in men are problems with the prostate. Prostatitis is a common urologic problem that is caused by an infection or inflammation of the prostate. This can cause pain in the area of the bladder, pelvis, anus and abdomen. Other prostatitis symptoms include painful urination, an urgent need to urinate and painful ejaculation.
Conventional Treatment
Pelvic pain treatment depends on the cause of the pain. Before pelvic pain can be treated, your doctor or health care provider will probably perform medical tests in order to determine the cause of pain. These tests may include lab work, a pelvic ultrasound, a pelvic MRI scan, a pelvic laparoscopy, a cystoscopy and a colonoscopy. These tests will give your doctor a much closer look at the organs in your pelvic area so that he or she can determine if there are any visible issues that may be causing the pain.
Research suggests that some potentially beneficial medications for pelvic pain include non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants and hormone therapy. For women with pelvic pain that’s associated with endometriosis or menstruation, hormonal treatment like birth control pills, gonadotropin-releasing hormone injections or progestin-releasing intrauterine devices are commonly prescribed.
In cases of severe chronic pelvic pain, surgery may be needed. Surgical procedures depend completely on the cause of the pelvic pain, but some common health problems that can be treated with surgery are fibroids, endometriosis and adhesions. A hysterectomy, which involves removing a woman’s uterus, is also a surgical option for very severe cases of pelvic pain.
Natural Treatments
1. Chiropractic Care
A 2015 case study published in The Journal of the Canadian Chiropractic Association found that chiropractic care was effective in reducing pelvic pain associated with pubic symphysis diatasis. This is when the pubic bones are separated or dislocated. In the study, a 30-year-old woman reported severe pelvic pain seven days after childbirth.
The pain was a constant, dull ache at the pelvic area with the pain becoming severe at times. The woman reported that the pain interfered with walking and lifting either leg. She also experienced pain at the lower back that radiated to both of her thighs.
Low-force chiropractic adjustments were done to several areas of the woman’s body, including the lower back, sacrum and the hip bones. Trigger points were identified and manual compression was applied to reduce tenderness.
The woman was also instructed on stabilizing therapeutic exercises, including Kegels, pelvic tilt and bridge and using a stability ball. Her pelvic pain improved immediately. After six weeks of chiropractic care, she reported progressive functional improvement and reduced difficulty standing up, walking, climbing stairs and lying on her side.
2. Pelvic Floor Physical Therapy
Physical therapy can help to relieve muscle pain and connective tissue pain. It can also help people with pelvic pain to learn how to strengthen, stretch, relax and control their pelvic muscles. Some pelvic floor exercises can help to reduce pain in the area by supporting the pelvic muscles, including the bladder, bowel and uterus. Some factors that cause the pelvic floor muscles to become weak are pregnancy, childbirth, obesity, lifting heavy objects and chronic coughing.
If your pelvic pain may be caused by weakened pelvic muscles, try doing Kegel exercises. These are done by contracting your pelvic muscles for 10 seconds and then releasing for 10 seconds. Repeat this series 10 times. Squatting and doing bridge pose can also be beneficial.
3. Biofeedback Therapy
Biofeedback is a type of training program that helps patients to control involuntary physiological processes that contribute to painful symptoms. This kind of therapy can be used to manage pain and tension, IBS, anxiety and many other health concerns that are triggered by chronic stress.
Research suggests that biofeedback therapy can be effective for pelvis pain because it prompts muscle relaxation and focuses on muscular re-education, which can provide symptom relief. Trained biofeedback therapists are able to determine how a patient’s symptoms can be minimized by learning to manipulate his or her involuntary physical behaviors. Patients can learn how to reduce muscle tension that leads to pain.
4. Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) is one of the most popular forms of psychotherapy that emphasizes the importance of underlying thoughts and how they make a person act or feel. For people who suffer from pelvic pain as a result of emotional stress or trauma, CBT or another form of psychotherapy can be extremely beneficial.
CBT gives patients more control over their lives and helps them to replace ways of living that do not work well with ways of living that have a positive, beneficial impact. Research shows that CBT can be helpful for patients with female sexual pain disorders. These disorders, which include vulvodynia and vaginismus, among others, can cause pain in and around the pelvic area, vagina, vulva and uterus. According to research published by the Association for Behavioral and Cognitive Therapies, one study found that almost 80 percent of women participating in CBT and physical therapy found relief from their pain.
5. Yoga
One of the many benefits of yoga is its ability to reduce pain and improve your quality of life. A 2011 study published in the Journal of Pediatric and Adolescent Gynecology found that yoga poses such as cobra, cat and fish poses, were able to reduce the severity of pain duration in women during their menstrual cycles.
Yoga poses also reduced the severity of pain and cramps. This study suggests that yoga can also be applied to pelvic pain treatment because it works to relieve pressure and manage gynecologic pain.
6. Acupuncture
Acupuncture stimulates specific points on the body in order to reduce pain and inflammation. Several studies show the usefulness of acupuncture for chronic pelvis pain in both men and women.
One study conducted in Japan found that pelvic pain decreased significantly after five acupuncture treatments. And further research supports the use of acupuncture to relieve pain in the pelvis and inflammatory reactions that can be contributing to the problem.
7. Anti-Inflammatory and High-Fiber Diet
Pelvis pain can be caused by a number of health conditions that involve inflammation, so sticking to a diet based on anti-inflammatory foods can be beneficial. Focus on eating plenty of antioxidant and omega-3 foods that will help to heal your body.
A 2013 study published in the Journal of Child Neurology found that the ketogenic diet works as a successful anticonvulsant therapy that can be used to relieve pain and inflammation. The ketogenic diet includes many anti-inflammatory foods, like leafy greens, carrots, broccoli, clean, organic protein, nuts, seeds, coconut oil and olive oil.
Research also shows that a high-fiber diet can be beneficial for people with pelvic floor disorders, especially when they are caused by digestive issues like constipation. Eating plenty of veggies, nuts and seeds can help to regulate your digestion and improve pelvic pain that’s caused by straining while using the bathroom or increased pressure on your abdomen and rectum.
In addition to eating these beneficial anti-inflammatory foods, stay away from foods that can make pain in the pelvic region worse. This include inflammatory packaged foods, artificially sweetened foods and beverages, excessive alcohol and refined carbohydrates.
8. Quercetin
Quercetin is a flavonoid antioxidant that helps to fight inflammation and free radical damage. Taking a quercetin supplement may help to treat the underlying cause of pain in the pelvis, especially if it’s caused by inflammatory conditions. A 2011 study published in The Urologic Clinics of North America found that quercetin was helpful for patients with organ-specific complaints involving the bladder or prostate, and pelvic floor spasms.
Quercetin supplements are available online and in many health food or vitamin shops. You can also get quercetin from foods like apples, peppers, blueberries, cherries, leafy greens, green tea, red wine and olive oil.
Precautions
There are many possible causes of pelvic pain and some of these conditions are serious. Make an appointment with your health care provider to determine the cause of your pain. Remember, pain in the pelvic region is a symptom and not a condition. So it can only be treated properly if you know what’s causing the pain in the first place.
If you are experiencing unusual pelvic region pain along with vaginal bleeding, call your doctor immediately, especially if you are, or may be, pregnant. This can be a sign of a miscarriage or gynecologic condition.
Final Thoughts
- Pelvic pain is continuous or intermittent pain that occurs in the pelvic area or lower abdomen. It causes the limitation of daily activities or a reduced quality of life.
- The worldwide prevalence of pelvis pain ranges between 5.7 and 26.6 percent.
- There are many possible causes of pelvic pain for both men and women. It can be caused by an infection, an issue with non-reproductive internal organs, like the colon or bladder, or for women, a problem with a reproductive organ. Stress or traumatic experiences, like sexual abuse, can also cause pelvic pain.
- Conventional treatment depends on the cause of the issue. Some common methods of treatment include NSAIDs, muscle relaxants and hormone therapy. In severe cases, surgery may be necessary.
- Natural treatments include chiropractic care, physical therapy and pelvic floor exercises, biofeedback therapy, cognitive behavioral therapy, yoga, acupuncture, anti-inflammatory diet and quercetin.








