This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Myositis: Causes of Inflammatory Muscle Diseases (+ 6 Natural Remedies)
August 22, 2018

Myositis is a general name for a group of conditions that cause muscle inflammation. The diseases are also known as inflammatory myopathies and can cause muscle weakness, pain and damage. In most cases, the disease responds to medical treatment.
Myositis is rare, and most people with this type of muscle inflammation require medical care. However, there are lifestyle and natural therapies you can use to possibly ease your symptoms.
What Is Myositis?
Myositis is an umbrella term for a group of muscle diseases that can cause inflammation and muscle damage. The inflammation affects muscles that you use to move, such as your arm, back, neck and leg muscles. There is technically no cure for myositis, but many people with an inflammatory myopathy achieve excellent control of their symptoms.
A myositis diagnosis may be made based on your symptoms, blood tests, an X-ray of your chest and lungs, electromyography (to check the electrical activity of your muscles), an MRI and a skin or muscle biopsy.
Signs and Symptoms
There are several types of myositis, and symptoms may vary among the diseases. Common symptoms for most forms of myositis may include:
- Feeling very tired or weak after standing, walking or climbing stairs
- Being clumsy, tripping or falling
- Difficulty swallowing or breathing
- Sore, weak or painful muscles after activity
- Weakness that gets worse over time (days to months)
More specific symptoms for each main category of myositis include:
- Polymyositis. Symptoms include muscle weakness on both sides of the body, starting with the trunk. Over time it causes increasing weakness. It can make it difficult to climb steps, stand up, lift things or reach above your head. Other symptoms include shortness of breath, arthritis or joint pain, trouble speaking or swallowing, and unusual heart rhythms. (1)
- Dermatomyositis. This disease is much like polymyositis, but it also has skin symptoms. A reddish or purplish rash may appear on the face, neck or chest, upper back and shoulders, knees, ankles, elbows and eyelids. The rash may be scaly, dry and rough. People with dermatomyositis may develop hard, painful bumps under the skin (calcinosis). They may also get tender little bumps under the skin from fat inflammation (panniculitis). Weakness mostly impacts the upper body, neck and thighs. Joint pain and inflammation (arthritis) may also occur. (2)
- Inclusion body myositis. This condition causes slow progression of muscle weakness that mostly impacts the thighs, wrists and fingers. It can also cause trouble swallowing. Many people with inclusion body myositis trip or fall fairly often. (3)
- Juvenile myositis. This disease affects children, although it may last into adulthood. It causes muscle weakness throughout the body. It can make it a challenge for patients to stand up from sitting, get dressed, comb their hair, climb stairs and do other activities. They may feel weak or tired often. In addition, most people with juvenile myositis get a rash. The rash is red or purplish, and is often found over the elbows, knees and knuckles. A purplish rash around the eyes is also common. The condition can also lead to hard bumps under the skin and trouble swallowing. (4)
- Necrotizing autoimmune myopathy. This type of myositis is rare and causes weakness in the upper and lower body. The onset of symptoms can be sudden, rather than gradual, and can become quite severe within just a few days or weeks. Other symptoms may include weight loss, muscle pain and fatigue. (5)
Causes and Risk Factors
Many cases of myositis do not have a clear cause. They happen when the body’s immune system starts to attack its own muscles, joints, blood vessels and connective tissues. These cases are considered autoimmune myositis. Toxic myopathies happen in reaction to medications.
In general, myositis causes may include: (5, 6, 7, 8)
- Viruses such as HIVH/AIDS, HTLV-1 or the Coxsackie B virus
- A temporary infection caused by a virus, fungus or bacteria
- Medications such as carticaine (an anesthetic), penicillamine (used to lower copper in the body), interferon-alpha (a cancer or hepatitis drug), cimetidine (ulcer medication), carbimazole (thyroid medication), phenytoin (a seizure drug), growth hormone and statin medications (prescribed for cholesterol)
- Allergic reactions to medicine or a toxic substance
- Injury
Risk factors for myositis vary by disease but may include: (5, 9)
- Age
- Polymyositis usually affects adults ages 30 to 60
- Dermatomyositis affects adults and children and is the most common myositis diagnosis in children
- Juvenile myositis primarily affects kids ages 2 to 15
- Inclusion body myositis is most common among adults 50 and older
- Necrotizing autoimmune myopathy can affect people of any age but is most common in adults
- Gender
- Polymyositis and dermatomyositis are more common among females
- Inclusion body myositis more commonly affects males
- Medication exposure to statins
- Treatment for cancer
- Diagnosis with HIV
- Other connective tissue diseases, such as lupus, rheumatoid arthritis, Sjögren’s syndrome and scleroderma

Conventional Treatment
Chronic forms of myositis cannot be cured. However, several types of myositis can be successfully treated so that symptoms are minimal or even gone for long periods of time (remission). Dermatomyositis and polymyositis typically respond the best, with juvenile and necrotizing diseases also having good success. Inclusion body myositis is considered the most difficult to treat due to the lack of known effective medication options.
According to the National Institutes of Neurological Disorders and Stroke, treatment for chronic inflammatory myopathies include: (5)
- Medication, such as high initial doses of corticosteroids.
- For people who do not respond to the first course of medication, immunosuppressant drugs may be given to reduce inflammation.
- Some people may receive periodic doses of immunosuppressant drugs to keep symptoms at bay.
- In cases that do not respond to the main drugs of choice, adrenocorticotropic hormone gel or biologic therapies may work.
- Note: There is no standard drug offering for inclusion body myositis. Corticosteroids and immunosuppressants often don’t work.
- Topical ointments for skin rashes and bumps.
- Protective measures for the skin, such as avoiding heavy sun exposure, wearing sunscreen and protective clothes, and even surgery to remove calcium bumps under the skin that cause pain or infection.
- Physical therapy to avoid muscle atrophy and maintain strength and flexibility
- Occupational therapy, orthotics and tools to assist with activities of daily living that may be challenging with myositis
- Targeted drugs for specific symptoms, such as trouble swallowing
Natural Remedies
Because myositis can be a chronic disease that gets worse over time, you should seek professional medical care for this condition. In addition, many people can benefit from at-home, natural symptom management and self-care. Work with your physician if you wish to incorporate these remedies into your care plan. Discuss with him or her any changes to diet, exercise, supplements or herbal remedies you would like to make, since natural therapies can interact with many drugs.
-
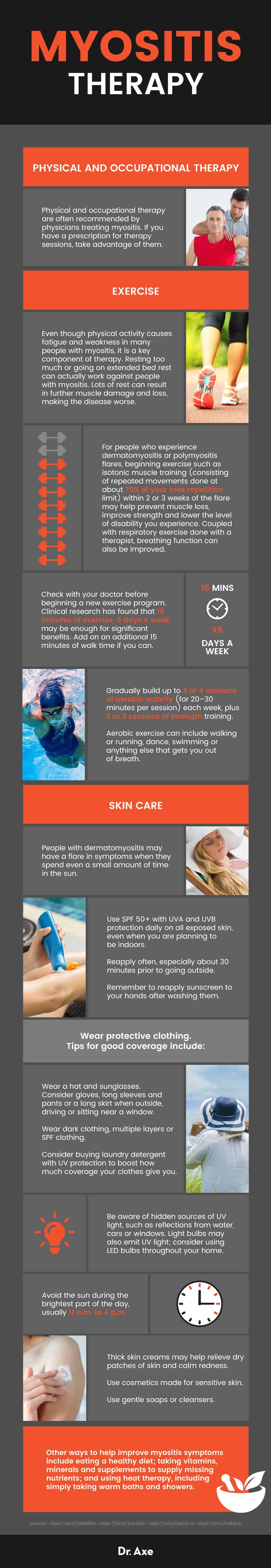
Make the most of physical and occupational therapy
Physical and occupational therapy are often recommended by physicians treating myositis. If you have a prescription for therapy sessions, take advantage of them. They provide personalized therapy that can make a major difference in how well you can function and take care of yourself. A few tips for making the most of these therapies include:
- Ensure that the therapist is familiar with your diagnosis or is willing to become familiar. Because myositis is rare and has many forms, even skilled therapists may not know about it prior to working with you. However, they should work to understand your disease and how it affects you by reading about it or speaking with your doctor. Once they are aware of which muscle groups are affected, how the inflammation impacts your symptoms, how well you function physically, and which activities you need assistance with, they should be able to craft a customized plan to make life more active for you.
- Speak up. If there are particular moves that cause pain or that are very difficult, the therapist can watch your form and help adjust your approach. Similarly, if there is something you want to learn or a way you want to improve your abilities, let them know. Therapists can target your sessions to accomplishing your main goals.
- Practice at home. Once you’ve had a session with a physical or occupational therapist, it is essential that you follow up with their recommendations at home. Without performing the exercises in between sessions, you may not see any improvement and your symptoms may even get worse.
- Think of therapy as an ongoing option. As you go through flares or as your disease progresses, physical and occupational therapy can be helpful again and again. With each change in your disease, these therapies can help you readjust. Ask for a referral from your physician any time you feel these therapies could help you.
-
Exercise and get strategic rest
Even though physical activity causes fatigue and weakness in many people with myositis, it is a key component of therapy. Resting too much or going on extended bed rest can actually work against people with myositis. Lots of rest can result in further muscle damage and loss, making the disease worse.
- Done correctly, exercise programs improve endurance and muscle strength and may reduce inflammation and disease activity. Exercise may be most useful when it involves intense resistance training. (10) Exercise may also: (11)
- Keep your disease from getting worse
- Help you lower doses of some medications
- Keep your clinical signs of disease stable
- Help you feel better about your health
- Help you make great gains in strength and endurance, especially if you are weak at the start of the program
- For people who experience dermatomyositis or polymyositis flares, beginning exercise such as isotonic muscle training (consisting of repeated movements done at about 70 percent of your max repetition limit) within two or three weeks of the flare may help prevent muscle loss, improve strength and lower the level of disability you experience. Coupled with respiratory exercise done with a therapist, breathing function can also be improved. (12)
- Check with your doctor before beginning a new exercise program. Clinical research has found that 15 minutes of exercise, five days a week may be enough for significant benefits. Add on an additional 15 minutes of walk time if you can. (11)
- Your program should include a warm-up and stretching to work on flexibility and range of motion.
- Exercise should emphasize strength training to help you maintain your muscle health. Think of resistance bands, light weights or using body weight for resistance.
- Gradually build up to three or four sessions of aerobic activity (for 20–30 minutes per session) each week, plus two to three sessions of strength training. Aerobic exercise can include walking or running, dance, swimming or anything else that gets you out of breath.
- Be sure you feel rested before exercising. However, do not go on bed rest unless told to do so by a physician.
- Rest after your workouts. You may wish to plan your exercise so that you can nap, relax or go to bed afterward. This gives your muscles time to repair themselves after each session.
- Take breaks throughout the day as you feel you need them. During a workout, rest when you feel you need to and continue when you’re ready. Rest before you get exhausted.
- Rest during acute flares. Take a break from your workout program for a few weeks so that you have time to recover.
- Rest the day before blood tests, since myositis and exercise can influence your creatine phosphokinase (CPK) levels. Tell your physician how recently you exercised before you got blood tests so they can better interpret your results.
-
Try heat therapy
Heat therapy can mean a wide range of treatments that focus on heating the muscles in a variety of ways. In many cases, physical therapists may recommend heat therapy after you do your exercises or when you feel tired or sore. Heat therapy is believed to relieve pain and relax muscles. It may also improve blood flow and ease swelling.
- The Johns Hopkins Myositis Center recommends whirlpool baths, heat packs and gentle massage for inflamed muscles. (13)
- The National Institute of Neurological Disorders and Stroke includes microwave thermotherapy and ultrasound therapies among appropriate treatments for dermatomyositis and polymyositis. (14, 15) Focused microwave therapy machines are used in many illnesses to either boost the effectiveness of medications or relieve pain. Ultrasound frequencies can be used to warm muscles, loosen tight muscles or joints and boost circulation. (16)
- Heat therapy recommendations for other immune-mediated inflammatory conditions, such as rheumatoid arthritis, include taking warm baths or showers, using moist or dry heating pads, or trying temperature-controlled paraffin baths. Paraffin baths may be most useful for people with pain or weakness affecting easy areas to dip in a wax bath, such as the wrist or ankle. (17)
-
Follow a myositis-friendly diet
In general, people with myositis need a balanced diet just like anyone else. However, the stakes are higher when your nutrition can directly impact symptoms and disease progression. People with myositis may benefit from some of these dietary tips recommended by physicians and clinical nutritionists at the Hospital for Special Surgery, which specializes in orthopedic conditions and musculoskeletal diseases: (18, 19)
- Get your grains. Grains such as brown or wild rice, whole wheat bread or pasta, oats, quinoa and corn offer fiber, energy and critical vitamins and minerals.
- Eat plenty of fruits, vegetables, beans, nuts and seeds. These offer a plethora of nutrients, antioxidants and fiber that are health powerhouses.
- Enjoy lean meat, fish and poultry. Trim fat and use healthy cooking techniques (roasting, baking, grilling) for about one serving of lean protein per meal.
- Focus on healthy fats and avoid solid fats, like lard or butter. Aim for olive, nut, seed or avocado oils. These are monounsaturated oils that are better for your health.
- Get plenty of calcium through dairy or dairy replacements. Calcium is critical for your bone and muscle health. Dairy products also offer zinc, selenium and vitamins that are important for your health. If you can’t digest lactose or you follow a vegan diet, opt for nut milks that contain calcium.
- Adjust your diet for medication side effects or disease symptoms. Many drugs have side effects that may respond to changes in diet. In addition, disease symptoms may be alleviated with dietary changes.
- Osteoporosis can be addressed by increasing your calcium and vitamin D intake. You can do this by adding dairy products or calcium-fortified non-dairy products to your daily diet. Alternatively, you can ask about calcium and vitamin D supplements to help protect your bone health.
- Swelling, fluid retention and high blood pressure are common side effects of myositis and certain drugs. You can consider a low-sodium diet, the DASH diet or just a simple limitation in how much sodium you consume. Frozen dinners, canned foods, lunch meat and many convenience foods often have high levels of sodium. Avoiding them can be an easy way to cut salt from your diet, reduce swelling and avoid heart and blood vessel complications caused by myositis.
- High blood sugar or diabetes caused by corticosteroids requires a diet lower in sugar and refined carbohydrates. Opt for whole grains and unsweetened foods and drinks. You should also have a nutritionist guide you on food choices to help with the adjustment to a diabetic diet.
- Weight gain and increased appetite can also be a side effect. Opt for low-fat and low-sugar snacks such as raw veggies and fruits, low-fat dairy products, whole grains and lean proteins. Monitor portion size. Eat smaller meals more often to satisfy your hunger without changing your overall calorie consumption too much.
- Decreased appetite and folic acid malabsorption can be common with the use of immunosuppressants. If you need a supplement for folate, take one. In addition, try eating green leafy vegetables as well as fortified cereals. If you have nausea, try avoiding greasy, acidic or spicy foods. Focus on dry foods such as cereal, bread or crackers.
- Get proper nutrition even with swallowing difficulties. If swallowing hurts or is challenging, let your doctor know. If the problem can’t be fixed, you may need to adjust your diet. Avoid malnutrition by asking about powdered supplements. You can also:
- Work with a speech therapist to learn ways to use your swallowing muscles differently.
- Purée or finely chop vegetables to use in healthy soups.
- Enjoy smoothies for breakfast and soft foods for snacks and other meals.
- Add healthy, high-calorie boosts to meals, such as peanut butter, yogurt, olive oil, cheese, puréed pumpkin or cooked fruit, oatmeal or applesauce.
- Avoid dry foods such as toast and crackers.
- Consider protein shakes that serve as meal replacements to make sure you get protein and calories.
-
Take care of your skin
People with dermatomyositis may have a flare in symptoms when they spend even a small amount of time in the sun. Since the symptoms can be severe, you should consider fairly significant sun protection measures if you have dermatomyositis. The Myositis Association recommends the following: (20)
- Use SPF 50+ with UVA and UVB protection daily on all exposed skin, even when you are planning to be indoors.
- Reapply often, especially about 30 minutes prior to going outside.
- Remember to reapply sunscreen to your hands after washing them.
- Wear protective clothing. Tips for good coverage include:
- Wear a hat and sunglasses.
- Consider gloves, long sleeves and pants or a long skirt when outside, driving or sitting near a window.
- Wear dark clothing, multiple layers or SPF clothing.
- Consider buying laundry detergent with UV protection to boost how much coverage your clothes give you.
- Be aware of hidden sources of UV light, such as reflections from water, cars or windows. Light bulbs may also emit UV light; consider using LED bulbs throughout your home.
- Avoid the sun during the brightest part of the day, usually 11 a.m. to 4 p.m.
In addition to being smart about sun exposure, you can care for dry or broken skin with some other at-home strategies: (21)
- Put coconut oil or a natural petroleum jelly alternative such as Waxelene or a similar ointment in a thick layer over sensitive or dry skin, such as the hands, and cover with cotton (such as cotton gloves or cotton clothing that you don’t mind using just for your skin care). Sleep with the skin covered and gently clean when you wake up.
- Thick skin creams may help relieve dry patches of skin and calm redness.
- Use cosmetics made for sensitive skin.
- Use gentle soaps or cleansers.
- Don’t cut cuticles that become thick or jagged. Instead, leave them alone and they should improve as your symptoms get under control.
-
Ask about supplements
Because myositis results in muscle damage, your body needs plenty of nutrients and building blocks for repairing tissue. Several vitamins, minerals and supplements may be helpful for people with myositis. Discuss their use with a health care professional before you begin, since some of these may interact with medication: (19)
- Creatine. Naturally found in proteins such as meat and fish, creatine is believed to help build muscle. Research shows it can improve muscle strength in myositis and other progressive muscle disorders. (22) It can also make a workout program more effective. (23) As a bonus, creatine may also improve how well you function and how well you feel. (24)
- Note: most research on this topic studied only short- and medium-term supplementation programs. Speak to a health care professional about ongoing supplementation.
- Fish oil. This popular supplement may reduce inflammation — a key marker in myositis. However, it may thin your blood and be dangerous if you take certain medications or need surgery.
- Calcium and vitamin D. Since corticosteroids and sun avoidance can both lead to deficiencies and osteoporosis in people with myositis, it’s critical to maintain your levels of calcium and vitamin D. Ask your doctor if you should take a supplement. You can also up your intake by consuming dairy products, wild salmon and bone-in sardines, enriched dairy alternatives, broccoli, kale and fortified cereals.
- Coenzyme Q10. People with inflammatory muscle diseases tend to have low levels of CoQ10. It’s unclear whether supplements may benefit people with myositis, but ask whether you should consider a supplement to get your levels into normal ranges.
- Glucosamine. This may help with cartilage, muscle, tendon and ligament repair. It may also reduce joint pain for people with arthritis, especially when taken together with chondroitin. However, this research is focused more on people with arthritis than those with myositis. Talk to a health care professional before adding glucosamine or chondroitin to your supplement regimen, especially if you don’t also have arthritis or joint pain.
- NOTE: Avoid spirulina, echinacea and green algae. These are considered immune system stimulants and may aggravate your disease. (25)
Precautions
- Many people with muscle pain, weakness and inflammation may get the wrong diagnosis. Evaluation at a specialized muscle disorders health center can ensure you know what causes your symptoms and how best to treat them.
- Myositis should be treated under the guidance of a medical professional. Do not attempt to self-diagnose or self-manage your care.
- Before changing your diet or exercise program, talk with a health care professional, physical therapist or occupational therapist who is familiar with myositis. Your program should meet your specific abilities, needs and goals.
- Do not start new vitamins, supplements or herbal remedies without consulting a health care professional. Many natural remedies can interact with medications and may cause side effects or health problems if your prescriber is not aware of what you take.
- Without proper treatment, most forms of myositis can progress to cause trouble swallowing, walking and taking care of yourself. Do not delay or avoid medical treatment or you may risk permanent muscle damage, falls, broken bones, malnutrition and other serious health complications.
Final Thoughts
- Myositis is a set of inflammatory muscle disorders. In most cases, the diseases cause muscle weakness, fatigue, inflammation and a gradual worsening in symptoms. Without treatment, the diseases can make it hard to walk, swallow and do many activities of daily living.
- Most forms of myositis are autoimmune-related. They can be triggered by infection or injury. Certain medications (such as statins) can also cause the condition.
- Medical options for myositis treatment generally include immunosuppressant drugs and corticosteroids. The drugs aim to reduce inflammation in the muscles and calm the immune system’s attack on muscle tissue.
- There is no cure for myositis, although most people with the disease have a good prognosis. Polymyositis and dermatomyositis are highly treatable and respond well to medication. Juvenile myositis and necrotizing autoimmune myopathy can also go away completely with therapy. However, many people may have flares of symptoms or may find their symptoms return when they stop treatment. Others, particularly those with inclusion body myositis, may not respond to any treatment.
6 Natural Ways to Help Myositis Symptoms
- Make the most of physical and occupational therapy
- Exercise and get strategic rest
- Try heat therapy
- Follow a myositis-friendly diet
- Take care of your skin
- Ask about supplements
