This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
7 Benefits of Natural Childbirth & 6 Steps for a Safe and Natural Childbirth
November 16, 2016
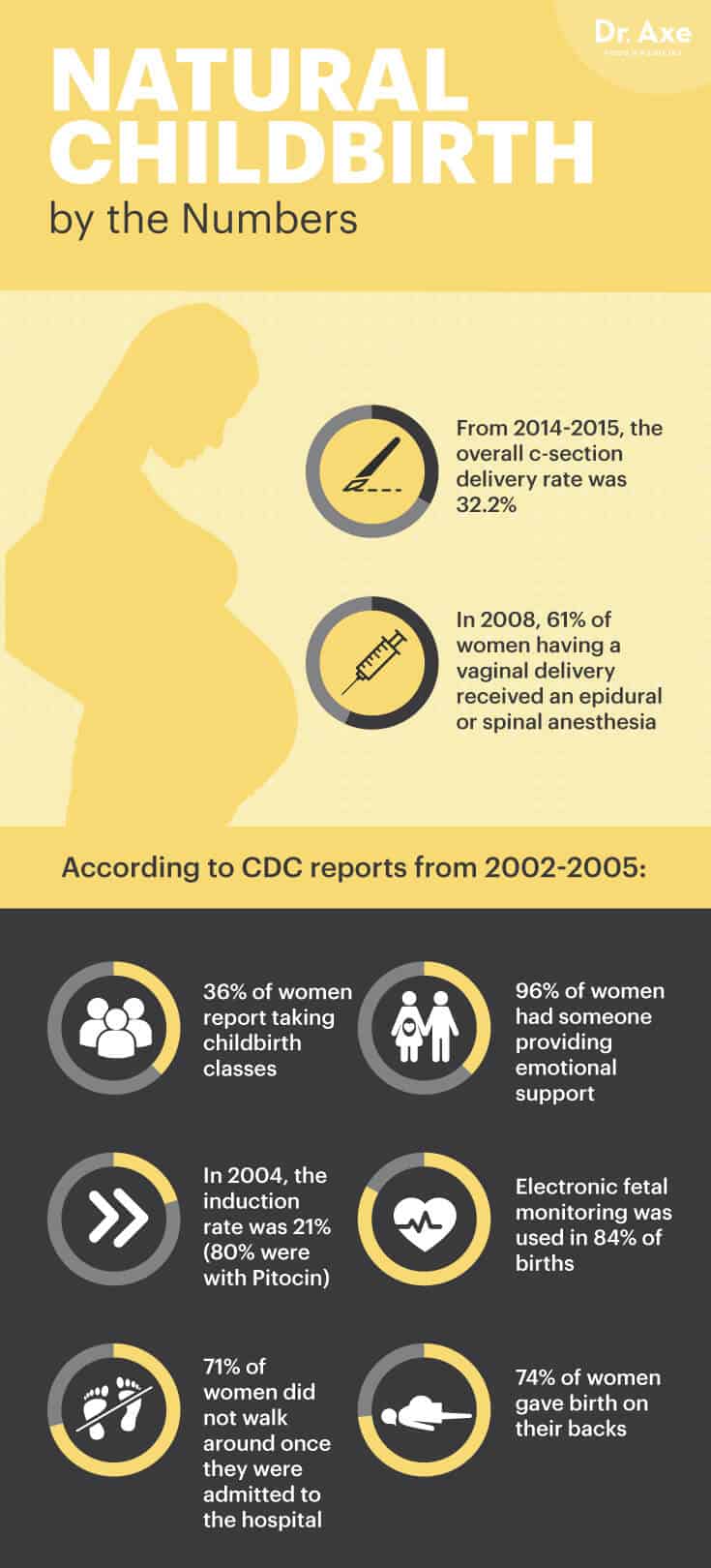
Research suggests that the way in which a woman experiences pregnancy and childbirth is vitally important for a mother’s relationship with her child and her future childbearing experiences. Unfortunately, we are currently in an era characterized by increases in obstetric intervention and cesarean section birth nationwide. With the U.S percentage of deliveries by C-section at 32.2 percent, now is the time for women to take control of their birth experiences through natural childbirth. (1)
According to Dr. Judith Lothian, who wrote “Why Natural Childbirth?” for the Journal of Perinatal Education, women are inherently capable of giving birth, have deep, intuitive instincts about birth, and when supported and free to find comfort, are able to give birth without interventions and without suffering. (2)
Choosing a natural childbirth, without interventions, allows a mother to feel completely in control of her birth experience and has many benefits for both the mother and baby.
What Is Natural Childbirth?
Natural childbirth is when a woman chooses to give birth using no medications or interventions. Instead, she uses techniques like controlled breathing and pain-relieving postures to deal with labor pains. With natural childbirth, the mother is in control of her body, and she is guided through the stages of labor with her chosen support system. Women who approach childbirth as a natural event end up feeling empowered by the experience, and research shows that women who feel in control while in labor feel more satisfied as a result.
According to research published in the Yale Journal of Biology and Medicine, natural childbirth is a system of intellectual, emotional and physical preparation for childbirth to ensure that mothers enjoy a healthier and happier pregnancy and delivery. (3) By choosing natural childbirth, women feel more in touch with the birth experience and better able to deal with labor in a proactive manner.
7 Benefits of Natural Childbirth (for Mother and Child)
1. Allows You to Avoid Interventions
The No. 2 benefit of natural childbirth is that you avoid the cascade of interventions that sometimes come with a conventional birth. Without becoming knowledgeable about coping strategies to deal with the pain, women end up opting for an epidural for pain management. When a woman has an epidural, a small amount of anesthetic is injected into the epidural space that surrounds the spinal cord. The anesthetic numbs the spinal nerves and blocks the pain signals, which lead to side effects. Common epidural side effects include a drop in blood pressure and fever.
Births also take longer when an epidural is used, and it may make it more difficult for some babies to get into the best position for birth. For this reason, research shows that when a woman has an epidural, the baby is more likely to need to be delivered with the help of instruments that use vacuum suction or forceps. (4)
An epidural is typically the first intervention during childbirth, and it may lead to more interventions being necessary. A woman’s body is designed to give birth naturally, and her hormones help facilitate childbirth. One of the most important hormones is oxytocin, which is responsible for stimulating contractions. Oxytocin helps labor progress naturally, but with an epidural, natural oxytocin production is inhibited, resulting in decreased plasma oxytocin concentrations.
Because epidurals typically slow the labor process, this leads to the next intervention — pitocin or syntocinon, which are synthetic forms of oxytocin. Sometimes pitocin is used to induce labor as well. A study published in the Journal of Clinical Anesthesia found that patients who have their labors induced request analgesia sooner and are at a higher risk of cesarean section than are patients who go into labor spontaneously. (5)
Cesarean section surgeries result in increased pain, including headache and backache, as well as increased risk of hemorrhage and uterine rupture. A C-section also results in greater risk of bladder injury and postpartum bladder infection or incontinence. C-sections also pose a risk to the baby. Researchers at the Ninewells Hospital and Medical School in the U.K. reported a 69 percent higher incidence of fetal deaths in C-section surgeries versus vaginal births. There is also a chance of fetal laceration, respiratory difficulties, inadequate transition to birth and increased incidence of mechanical ventilation. (6)
2. Lets You Move Around Freely
Lying on your back during labor can result in poor quality contractions, dystocia, slow dilatation and effacement, prolonged labor, and failure to descent. The result of laboring while lying on your back increases the rate of C-section surgeries because of fetal distress or failure to progress or descent. Unfortunately, bed rest is required after an epidural because the woman’s legs are numb and she is a fall risk, and women must be monitored to be sure the baby’s heart rate isn’t dropping. In addition, bed rest can cause more pain, necessitating additional pain medications.
Research shows that unrestricted movement during labor allows the mother to find a position that’s more comfortable for her. It’s been found to decrease maternal pain, facilitate maternal and fetal circulation, increase the quality of uterine contractions, and facilitate fetal descent. Positions such as the knee-chest can reduce back pain related to posterior fetal position, and the use of the shower or bath can aid pain relief. (7)
3. Allows You to Eat and Drink
Research from the American College of Nurse-Midwives indicates that the lack of nutritional support during labor can cause maternal dehydration, ketosis, hyponatremia and increased maternal stress. Women who give birth naturally at a birthing center or hospital are able to eat and drink freely, which sustains their energy levels during labor.
4. Initiates Breast-Feeding More Easily
An infant may be impacted by labor and birth medications in a way that impairs launching breast-feeding. The natural process of labor and birth prepares both mother and baby for breast-feeding. Birth practices including induced labor, routine interventions, epidurals and separation of mother and baby disrupt the process of early breast-feeding.
Research shows that the way the birth proceeds powerfully influences the first hours and days of breast-feeding. Normal, natural birth sets the state for problem-free breast-feeding, while complicated, intervention-intensive labor and birth set the stage for difficulties with breast-feeding. (8)
5. Makes You Feel in Control
It’s well-known that a woman’s sense of control during childbirth is related to a positive birth experience. In a concept analysis, the idea of control during childbirth was evaluated. Researchers found that women mostly described control in relation to bodily function and pain. Their ability to handle pain and other difficulties was a source of satisfaction that contributed to their positive experiences. The experience of control made it easier for the women in labor to turn their focus inward, letting go of the outside world.
When a woman feels like she took command of her birth, this makes her feel more capable of giving birth naturally, and it gives her a sense of empowerment. And after the birth, she feels proud of the experience. Even if you end up needing some kind of intervention, the fact that you are a part of the decision and in control of your experience contribute to your positive memory of the birth. (9)
6. Gets Your Partner Involved
According to a 1999 study published in Midwifery, support provided by the male partner during childbirth evoked very positive responses from the women participants. A natural childbirth allows your partner to get involved in the process by helping you carry out pain-relieving positions. (10) Simple strategies like applying pressure to your lower back and hips during a contraction, standing and leaning against you so you can sway back and forth, and counting for you in the pushing stage bring you and your partner closer during the birth experience.
7. Improves Baby’s Gut
Researchers at Columbia University suggest that disrupting the mother-to-newborn transmission of bacteria by C-section delivery may increase the risk of celiac disease, asthma, type 1 diabetes and obesity in the child. During a vaginal delivery, bacteria colonize the infant gut, and after birth, breast milk promotes the colonization and maturation of the infant gut microbiome. This is important because it helps the infant develop a strong immune system.
Because childbirth with interventions are more likely to lead to a C-section delivery, a natural childbirth ensures that your baby passes through the vaginal flora and relieves healthy bacteria. (11)
6 Steps to Take for a Safe and Natural Childbirth
1. Find Support
On the big day, it’s so important that you have the right team by your side. Find a supportive health care provider who is comfortable with your plan to give birth naturally. Look for a midwife or doctor who agrees with your perspective and ensures you that he or she will take all measures to avoid intervention unless absolutely necessary.
It’s common for women seeking natural childbirth to use a midwife, and research shows that midwives provide one-to-one delivery care and continuous attendance when at the bedside of delivering women, which have positive effects on birth outcomes. (12) Recently, midwives are playing a prominent role during childbirth in many hospitals as the first-line hospital provider or as a part of a team with physicians. (13) That means that you don’t have to give birth at home or in a birthing center to benefit from midwifery care.
A doula also serves as a supportive birth coach who is strictly there for you. A doula stays by your side in the delivery room and serves as the rock that you need, especially if you wish to give birth naturally.
A 2013 study found that expectant mothers matched with doulas had better birth outcomes. Doula-assisted mothers were four times less likely to have low birth weight babies, two times less likely to experience birth complications involving themselves or their babies, and significantly more likely to initiate breast-feeding. Researchers also indicate that communication with and encouragement from a doula throughout the pregnancy may have increased the mother’s self-efficacy regarding her ability to impact her own pregnancy outcomes. (14)
2. Pick the Perfect Environment for You
When it comes to picking the location of your childbirth, you have options. You can research hospitals with low C-section rates in your area and go on tours to see if you feel at ease in the space. Many women prefer to give birth in a hospital because it feels safe and comforting to have the appropriate equipment and medical team in case an intervention is needed. But do consider your options before automatically choosing to give birth in a hospital.
Research published in Midwifery Today with International Midwife suggests that planning a hospital birth is not safer than planning an attended home birth for women with one head-down fetus, between 37–42 weeks, no high blood pressure, no previous caesareans and no serious medical conditions that affect pregnancy outcomes. (15)
You can also look into local birthing centers, which are becoming more and more popular. A birthing center is a home-like setting where care providers, usually midwives, provide family-centered care to healthy pregnant women. Most birth centers are located separately from hospitals, and some are physically inside of the hospital building. The benefit of giving birth in a birthing center is that women are allowed to make their own decisions regarding the circumstances of their births. Women are encouraged to eat if they’re hungry (which isn’t typically allowed in a hospital), move around, spend time in a tub if they wish and choose the positions that make them feel comfortable.
A 2013 study published in the Journal of Midwifery and Women’s Health shows that birth centers provide first-rate care to healthy pregnant women in the U.S. Of the 15,574 women who planned and were eligible for birth center birth at the onset of labor, 93 percent of them had spontaneous vaginal births, 1 percent had assisted vaginal births and 6 percent had cesarean births. (16)
Another option is a planned home birth. While the number of women in developed countries who plan home births is low, it has increased over the past decade in the United States. In 1938, 50 percent of women in the U.S. had home births, and that number dropped to fewer than 1 percent in 1955. Hospital births became the cultural norm in the later years of the 20th century, but the numbers are slowly beginning to increase again.
According to research published in the International Journal of Women’s Health, the benefits of planned home birth include lower rates of interventions and maternal morbidity. Women who have planned home births have high rates of satisfaction related to home being a more comfortable environment and feeling more in control of the experience. (17)
3. Prepare Yourself Physically
Labor has been defined as “powered by the innate human capacity of the woman and fetus.” It’s within a woman’s physical capabilities to give birth to a baby, but that requires some preparation beforehand. While in labor, you respond to the pain of uterine contractions by moving around. Movement is a coping strategy for pain, and the freedom to be mobile in labor is very important.
According to research published in the Journal of Perinatal Education, women who use upright positions and are mobile during labor have shorter labors, receive less intervention, report less severe pain and describe more satisfaction with their childbirth experiences than women in recumbent positions. (18)
To prepare yourself for a natural childbirth that will require you to change positions throughout the course of your labor, stay physically active during your pregnancy. Long walks, yoga and light weight-lifting during your pregnancy help boost your endurance and flexibility while in labor. Prenatal yoga can be especially helpful because you can use the same positions to open up the cervix and relieve pain during a natural childbirth — plus, yoga changes your brain and helps you relieve anxiety and feel more in control.

4. Take a Class
Women with proper education and preparation can be taught to give birth naturally. Although childbirth is a natural occurrence and women are born with this ability, it certainly helps to be prepared with coping strategies on the big day.
During your pregnancy, take a class or course that focuses on natural childbirth. This helps prepare you and your partner by solidifying your birth plan and giving you the tools to get through labor without intervention. A 2012 study found that attending prenatal education classes was associated with higher rates of vaginal births among women in the study sample. (19)
The Bradley Method is a popular form of natural childbirth that uses the help of a coach/advocate along with various pain-reducing techniques to help moms deliver their babies without unnecessary interventions or drugs. The method is usually taught over the course of 12 weeks through childbirth classes that ideally involve both mother and father (or another person who acts as the birching “coach”). Taking a course like this encourages you to learn to trust your body and rely on natural methods for birthing.
5. Stay Nourished
Poor nutritional balance may be associated with longer and more painful labors. In most hospitals today, women are not allowed to eat or drink water while in labor incase they have to be given general anesthesia. Since the 1940s, it’s routine practice to prohibit food and drinks during labor because during general anesthesia, there is an increased risk of the stomach contents entering the lungs. With better general anesthesia techniques, these rules may no longer be necessary, but many hospitals haven’t changed their protocols. (20)
This is one reason why giving birth at a birth center or at home may be a better option for you. If you choose to give birth at a hospital, labor at home for as long as possible first, and be sure to drink plenty of water at that time. Before going to the hospital, eat a well-balanced meal or drink a smoothie if you’re in too much pain to eat. In the days leading up to your due date, stay hydrated and stick to a healthy and well-balanced diet to be sure that you’re well-nourished for labor.
6. Stay Positive
Every woman’s birth experience is different, and it’s important to remember that you will write your own birth story. That’s why you shouldn’t compare yourself to other women and their experiences. You will hear plenty of horror stories about emergency C-sections and vacuum extractions, but this mind-set will only hinder your ability to stay strong in the delivery room.
Politely disregard the naysayers, and focus on positive thoughts leading up to your due date. Even establishing a mantra or prayer to focus on during childbirth can be helpful. Mantras such as “I am powerful” or “my body knows what to do” can help you remain focused during a contraction.
Something to Remember with Natural Childbirth
Sometimes a mother experiences feelings of failure and guilt when she planned a natural childbirth but ended up using interventions. A 2001 study conducted at Harvard Medical School found that 88 percent of the participants who chose natural childbirth but ended up requesting an epidural for pain reported being less satisfied with their childbirth experiences than those who did not, despite lower pain intensity. (21)
Remember that each woman’s birth experience is different and planning a natural childbirth proves that you’re focused on providing the healthiest experience for your newborn. If an intervention becomes necessary, you should be proud that you were able to stay in control of your birth experience and make important decisions for your family.
Final Thoughts on Natural Childbirth
- Research suggests that the way in which a woman experiences pregnancy and childbirth is vitally important for a mother’s relationship with her child and her future childbearing experiences.
- Natural childbirth is when a woman chooses to give birth using no medications or interventions. Instead, she uses techniques like controlled breathing and pain-relieving postures to deal with labor pains.
- Some benefits of natural childbirth include avoiding interventions (many of which have side effects), initiating breast-feeding more easily, feeling more in control of your experience, boosting the baby’s immune system by providing healthy bacteria through the vaginal flora, and getting your partner more involved.
- Some steps to take in preparing for a natural childbirth include finding a supportive team, choosing the right environment for you, getting physically and mentally prepared, taking a class, moving around while in labor, and being well-nourished.








