This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Ear Infection Symptoms, Causes & Risk Factors to Avoid
October 31, 2016

Wondering if your painful symptoms are pointing to an ear infection and what you should do to help these potential ear infection symptoms go away?
Symptoms of ear infections usually include earaches or throbbing pain, sometimes a fever, and signs of inflammation near the ears like redness or fluid leaking out. Although antibiotics are assumed to be the treatment of choice for ear infections, you might want to reconsider this approach. According to the Institute for Quality and Efficiency in Health Care, “The majority of middle ear infection cases will usually clear up on their own within a few days, with or without treatment. The main aim of treatment is to relieve the symptoms (relieve pain and reduce fever)… Antibiotics only slightly influence the course of middle ear infections, and they can have side effects.” (1)
Another surprising finding about using antibiotics to treat ear infection symptoms? While about 80 out of 100 children (80 percent) who take antibiotics no longer have earaches after two to seven days, 70 out of 100 (70 percent) who don’t take any antibiotics have the exact same results. That means antibiotics only help about an additional 10 percent of the population who suffers from earaches. Plus, side effects of antibiotics can sometimes include nausea, diarrhea and skin rashes, in addition to altering gut health and possibly contributing to future infections.
What are some natural ear infection remedies that can help curb symptoms without the use of antibiotics? These can include applying a warm compress, reducing allergies, boosting immunity through use of certain herbs and/or supplements, and applying antibacterial essential oils to the ear.
What Is an Ear Infection?
Ear infections occur whenever bacteria or a virus affects any part of the ear and causes inflammation. This can occur in the outer, middle or inner parts of the ears. There are several different types of common ear infections that affect both children and adults. Two of the most common are:
- Middle ear infection: Acute middle ear infections are commonly referred to by doctors as acute otitis media. They affect children commonly and include the type of ear infection called swimmer’s ear. (2)
- Inner ear infections: These are much rarer than middle ear infections. Doctors refer to inner ear infections as vestibular neuritis and labyrinthitis. These are infections that inflame the inner ear or the nerves connecting the inner ear to the brain, causing ear infection symptoms like sensory disruption, hearing problems, vertigo and dizziness.
Are ear infections contagious?
Ear infections can be both bacterial or viral in nature. They’re usually not contagious, however some that are bacterial can be. For example, if someone develops swimmer’s ear from swimming in water contaminated with harmful bacteria, then the bacteria itself are contagious. However, most ear infections are not contagious because they’re symptoms of people’s own immune responses (much like allergic reactions). (3) Similarly, if an ear infection is caused due to a virus or another illness, the viral/illness itself is likely contagious but not the infection of the ear itself.
Ear Infection Symptoms and Signs
- Earaches and ear pains: Symptoms can feel like throbbing or pulsing in the ears, especially with movement or during sleep.
- Trouble sleeping due to ear pain: Especially when sleeping on one’s side and pressing against the head or ear.
- Fever symptoms: Fevers can sometimes become high in young children (over 100.5 degrees F or 38 degrees C). Fever symptoms can include high temperature, chills or sweats, dizziness, upset stomach, loss of appetite, vomiting, muscle aches, and fatigue.
- A red, inflamed eardrum: Your doctor might be able to observe this when looking into the ear canal. Sometimes the eardrum can even bulge out and feel stiff if it becomes very swollen with backed-up fluid.
- Itchiness in the ear.
- Pain around the ears, radiating down the neck and side of the head.
- Crying, head shaking and rubbing in children: Because many small children aren’t sure what the source of their pain is or can’t identify exactly where it’s coming from, some tend to rub and shake their heads, stomachs or ears a lot. Babies or children with ear infections also usually become irritable, cry more and become restless at night.
- Sometimes signs of a head cold: Coughing, sneezing and a stuffy nose can be related to ear infections because all are caused by swelling in the mucous membranes, which leads to trouble breathing normally in some instances. Sometimes nasal sprays or lozenges/decongestants are used to open the airways, however this doesn’t usually help the actual infection to go away.
- Fluid leaking from the ears: Sometimes ear infections cause thick, sticky fluid to be secreted. Fluid might be clear or mixed with pus and blood. Fluid and pus behind the eardrum is called effusion, and leaking of fluid from the ear is called otorrhea.
- With inner ear infections, sensory changes can occur, including hearing changes, dizziness, loss of balance, nausea and vertigo.
Can ear infections cause long-term complications?
Only in rare cases does an infection of the ears progress for more than one to two weeks, in which case treatment from a doctor is necessary in order to prevent complications. Some long-term ear infection symptoms can include:
- Hearing complications: In severe cases, the ear infection might cause the mucous membranes to swell up and secrete fluid for several weeks even after the initial infection subsides. This is called otitis media with effusion (OME), also known as glue ear, which is caused by the tympanic cavity filling up. This occurs most often in middle ear infections and usually clears on its own, however if it persists for more than several days and the infection is left untreated, sometimes changes in hearing and balance can occur.
- Although it’s rare, ear damage that causes hearing changes can sometimes contribute to speech delays and other developmental language challenges if the child is never treated to overcome this condition.
- Mastoiditis: This is a bacterial infection of the membranes lining the mastoid bone, a bone in the skull that’s located close to the ear. When left untreated it can result in permanent damage.
- Meningitis: Another infection of the membranes covering the brain and spinal cord, which can cause nerve damage, pain, very high fevers and bacteria to spread to bone.
Ear Infection Causes and Risk Factors
Children under 6 years old develop ear infections most often, especially if they spend a lot of time near other children in day care centers, do a lot of swimming in pools or outdoors, or if they have allergies.
There are several general causes for ear infections:
- Many ear infections begin as someone is overcoming another infection or illness, especially a cold, respiratory infection, virus or the flu. This can cause more fluid and bacteria than usual to accumulate in the mucous membranes, which wind up backing into the ear canal. In the case of a middle ear infection, it’s been found that other illnesses cause inflammation of the membranes lining the Eustachian tube in the ear (the canal that connects the middle ear to the throat area) and trap fluid.
- Swimmer’s ear is another ear infection caused from water and bacteria getting trapped inside the ear canal, usually due to the buildup of wax. Bacteria can either enter the ear canal through water and then get trapped inside, where they can proliferate and cause infections, or someone’s own “normal bacteria” can become trapped.
- Ear infections are also caused by allergies, especially middle ear infections. Allergies can affect the entire upper respiratory system and lead to infection because they cause fluid to build up in the ear (sometimes which also winds up leaking out).
Why do children and babies get ear infections more often than adults do? Children have shorter and narrower Eustachian tubes in their ears than adults. This allows them to become inflamed and clogged with fluid more easily. Children also experience more pain from ear infection symptoms because the nerves in their ears tend to be more sensitive.
Other than being a child, risk factors for developing ear infections include:
- Having genetically enlarged polyps that block the middle ear and can trap fluid or bacteria.
- Suffering from seasonal allergy symptoms or food allergies (this can include celiac disease, hay fever allergies, etc.).
- Suffering from other conditions that affect the ears, such as sinusitis.
- In children or babies, using a pacifier, going to day care or being formula-fed. Breastmilk is known to increase immune function in infants because it supplies crucial nutrients and antibodies needed to defend against foreign microbes. (4)
- In regard to developing swimmer’s ear, frequent swimmers, surfers, divers and other individuals who are exposed to wet and warm conditions are at an increased risk for recurring infections. (5)
- Smoking cigarettes or using other drugs that are toxic and hinder immunity. Smoking around children (exposing them to secondhand smoke) has been shown to increase their risk for ear infections. (6)
- Swimming in contaminated water that can contain bacteria.
- Any other lifestyle habits that lower immune function, such as alcoholism, having an autoimmune disorder, a lack of sleep, taking immune-suppressing drugs and even being overly stressed.
Conventional Treatment for Ear Infection Symptoms
Few parents are aware that antibiotics aren’t always necessary or even helpful at all in treating their children’s ear infections. (7) Most ear infections are actually caused by viruses, not by bacteria. The exception is in children under the age of 2, if an infection develops after swimming in potentially contaminated water or if there is visible fluid leaking from the ear. In these cases, the infection is likely due to bacteria.
So although antibiotics might be helpful and necessary in some cases to treat bacterial ear infection symptoms, they’re often overused. And this doesn’t come without potential risks. Antibiotics can contribute to nausea, skin rashes, changes in gut health and even lowered immune function overall. A better way to manage ear infections is due to focus on preventing them from happening in the first place and then reducing pain with things like heat and essential oils while waiting and watching the infection.
Prevention and Natural Treatments for Ear Infection Symptoms
1. Reduce Ear Pain Naturally
Children and adults dealing with infections who are in pain can take or be given low doses of an over-the-counter painkiller (such as acetaminophen or ibuprofen) to reduce inflammation/swelling and throbbing. These can also help lower a fever and symptoms like having the chills or dizziness. This “wait and see” approach is considered by many experts to be a better and safer approach than overusing antibiotics. A heated compress, warm shower or heating pad used when sleeping that are applied to the affected ear or side of the head can also be helpful.
Of course, be careful not to overdo it and rely on prescription painkillers, which can lead to acetaminophen overdose or ibuprofen overdose. In fact, it’s best to start with natural painkillers to see if they work, preventing any potential side effects from pain-relieving pills.
2. Breast-Feed Infants to Increase Immunity
Research shows that breast-fed babies are less likely to have ear infections — in addition to many related problems like allergies, respiratory infections, pneumonia, bronchiolitis and viral infections, such as meningitis. Breastmilk can build a child’s immune system by supplying needed nutrients, calories, growth factors and fluids necessary for development, plus transmit immunoprotective substances from the mother to her child that formulas don’t have.
3. Reduce Allergies and Inflammation with a Healthy Diet
Certain dietary changes might be able to help reduce allergies and respiratory inflammation along with increasing immunity against infections, including:
- Reduce intake of inflammatory foods, including packaged, processed foods, added sugars, and common allergens like conventional dairy, gluten, shrimp and peanuts.
- Consume more veggies and fruits, garlic, ginger, turmeric and other spices/herbs, water, wild-caught fish and other “clean” proteins, and probiotic foods.
- Also consider taking helpful supplements, such as omega-3 fish oils, probiotics, zinc, vitamin C and helpful antiviral herbs like calendula, elderberry, astragalus and echinacea.
4. Prevent Inner Ear Moisture with Ear Drops
Most drug stores carry over-the-counter ear drops that can help dry up moisture inside the ears in people who are susceptible to reoccurring ear infections or earaches due to swimmer’s ear. Not removing natural earwax, protecting the ear canal with plugs when swimming or applying a homemade wax substitute in the ears can also help prevent swimming-related infections.
How Common Are Ear Infections?
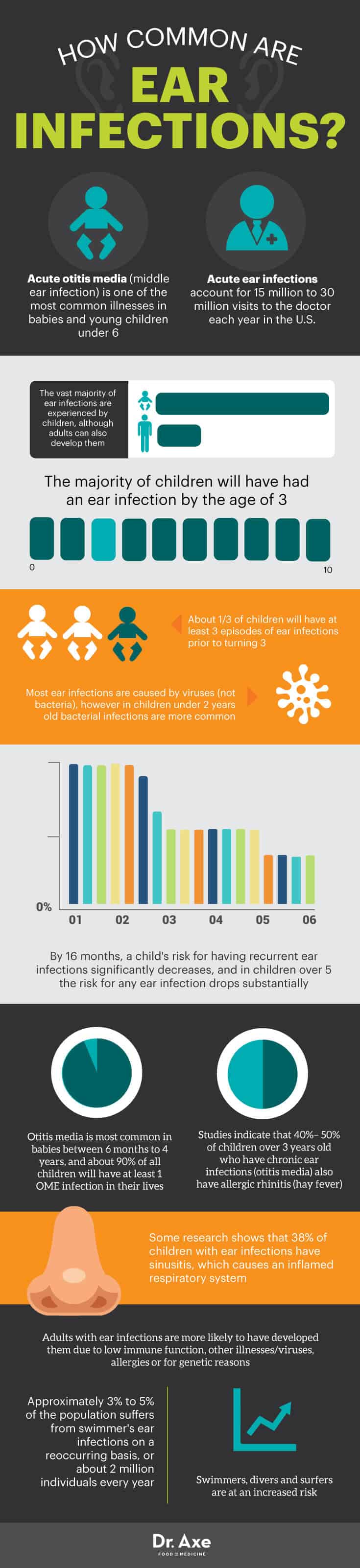
- Acute otitis media (middle ear infection) is one of the most common illnesses in babies and young children under 6. Acute ear infections account for 15 million to 30 million visits to the doctor each year in the U.S. (7) The vast majority of ear infections are experienced by children, although adults can also develop them.
- The majority of children will have had an ear infection by the age of 3. (8) About one-third of children will have at least three episodes of ear infections prior to turning 3.
- Most ear infections are caused by viruses (not bacteria), however in children under 2 years old bacterial infections are more common.
- By 16 months, a child’s risk for having recurrent ear infections significantly decreases, and in children over 5 the risk for any ear infection drops substantially.
- Otitis media is most common in babies between 6 months to 4 years, and about 90 percent of all children will have at least one OME infection in their lives.
- Studies indicate that 40 percent to 50 percent of children over 3 years old who have chronic ear infections (otitis media) also have allergic rhinitis (hay fever).
- Some research shows that 38 percent of children with ear infections have sinusitis, which causes an inflamed respiratory system.
- Adults with ear infections are more likely to develop them due to low immune function, other illnesses/viruses, allergies or for genetic reasons.
- Approximately 3 percent to 5 percent of the population suffers from swimmer’s ear infections on a reoccurring basis, or about 2 million individuals every year. Swimmers, divers and surfers are at an increased risk.
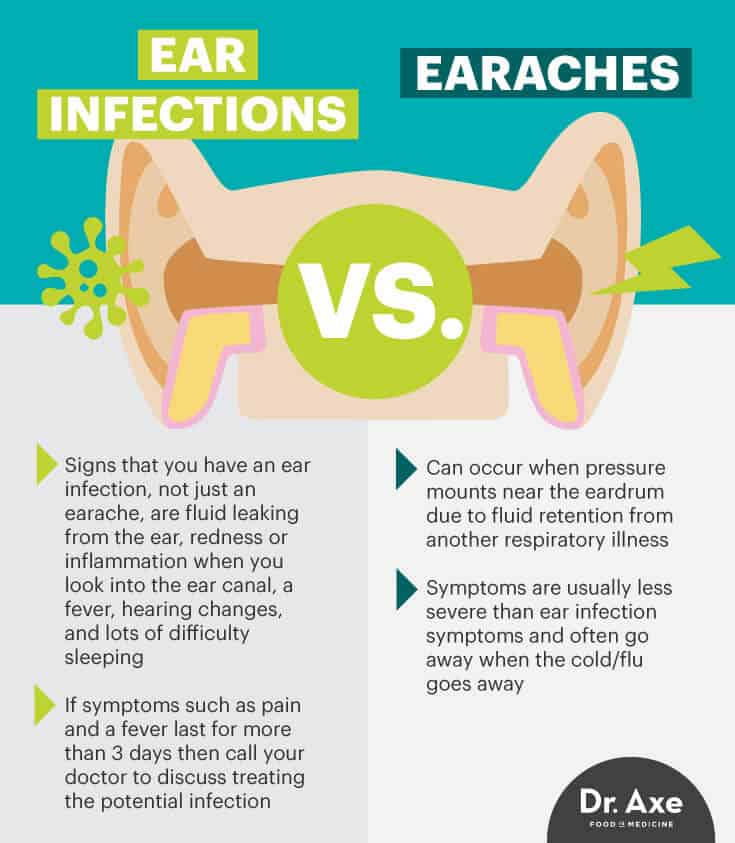
Ear Infections vs. Earaches: How to Tell the Difference
- Earaches can occur when pressure mounts near the eardrum due to fluid retention from another respiratory illness (such as a common cold or the flu). Earache symptoms are usually less severe than ear infection symptoms and often go away when the cold/flu goes away.
- Signs that you have an ear infection, not just an earache, are fluid leaking from the ear, redness or inflammation when you look into the ear canal, a fever, hearing changes, and lots of difficulty sleeping.
- Most earaches go away on their own and don’t require treatment, but if symptoms such as pain and a fever last for more than three days, then call your doctor to discuss treating the potential infection.
Precautions Regarding Ear Infection Symptoms
If an ear infection develops in your young child or toddler, closely monitor signs of the infection, such as pain and throbbing. This is especially important in infants, who should be examined by a doctor. Head to your doctor if ear infection symptoms don’t subside within two to three days.
In children, infections of the ears can sometimes (although rarely) cause inner ear damage that can lead to changes in hearing. So look out for any signs of hearing loss, and discuss anything unusual you notice with your doctor right away. If you do give your child a low dose of an over-the-counter painkiller to reduce symptoms, be careful not to use aspirin. Aspirin has anti-inflammatory effects but isn’t always well-tolerated by children and teenagers, so use ibuprofen unless a doctor has prescribed another drug or — preferably — natural pain relievers if you can.
Final Thoughts on Ear Infection Symptoms
- Ear infections are bacterial or viral infections that cause inflammation in the outer, middle or inner parts of the ears. The most common type of ear infection, especially in young children or babies, is middle ear infection (also called acute otitis media).
- Children under 3 years old are most likely to develop ear infection symptoms, which normally include throbbing near the years, difficulty sleeping, and sometimes a fever or fluid leaking from the ear.
- Risk factors for ear infections include recovering from another respiratory illness, having allergies, being near other sick children, eating an inflammatory diet, and being exposed to secondhand smoke or contaminated water.
- Natural remedies for ear infection symptoms include applying a warm compress to the ears, using an over-the-counter painkiller or natural painkiller when necessary, improving gut health/immunity through dietary changes, and reducing moisture trapped within the ear.


