This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
What Is Ascites? (+ 6 Natural Ways to Manage Ascites Symptoms)
September 25, 2023

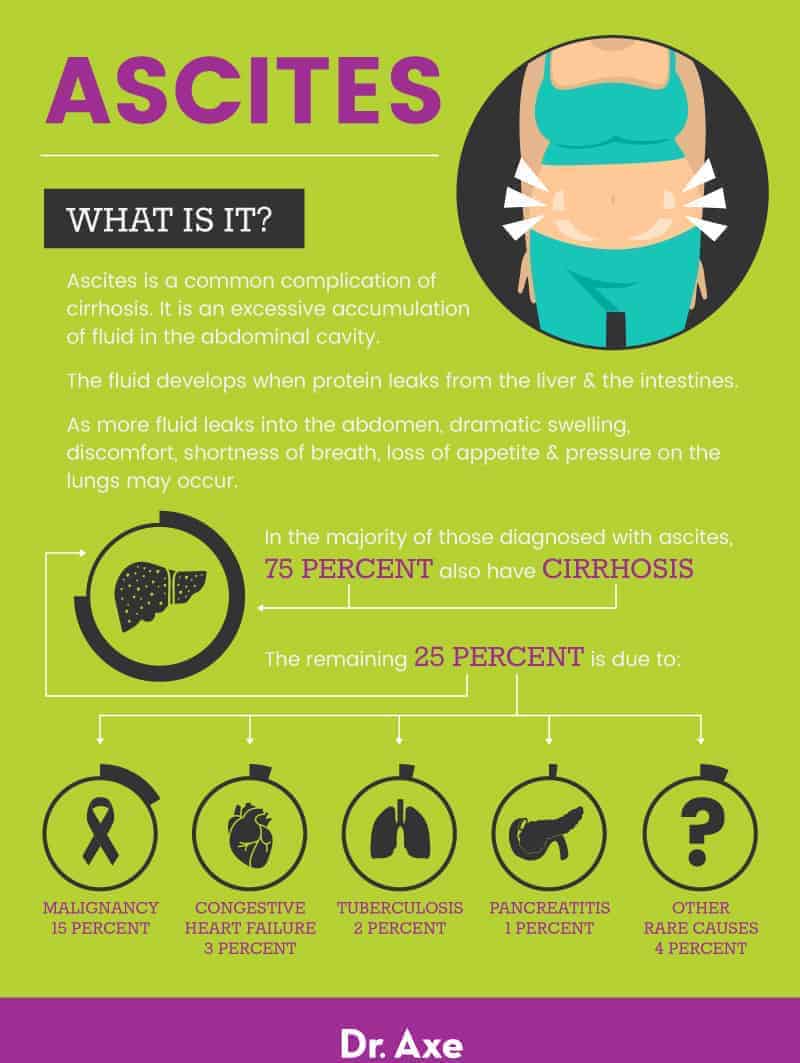
Ascites is the accumulation of fluid within the abdomen. While there are a number of conditions that can cause it, approximately 75 percent of patients with ascites also have cirrhosis of the liver. In addition, about 50 percent of patients with cirrhosis will develop ascites within 10 years.
It is considered a frequent complication of end-stage liver disease as well as other fluid retention conditions, including pleural effusions and peripheral edema. Ascites significantly impacts quality of life.
There is no cure, but conventional and natural treatments for ascites can help relieve symptoms, including pain and discomfort.
What Is Ascites?
Ascites is a common complication of cirrhosis and is marked by an excessive accumulation of fluid in the abdominal cavity. Generally speaking, fluid retention — including ascites, peripheral edema and pleural effusion — is the most frequent complication of end-stage liver disease.
In approximately 15 percent of cases ascites is caused by certain types of malignancies in the gastrointestinal tract or in the ovaries, Hodgkin’s lymphoma, non-Hodgkin’s lymphoma, and metastatic carcinoma in the abdominal cavity. It is also linked less often with heart failure, tuberculosis, pancreatitis and even hypothyroidism.
The fluid in the abdominal cavity develops when protein leaks from the liver and the intestines. If it is just a small collection of protein-rich fluids, it may be difficult to detect. However, as more and more fluid leaks into the abdomen, dramatic swelling, discomfort, shortness of breath, loss of appetite and pressure on the lungs may occur.
There are two main types of ascites: uncomplicated and refractory.
Uncomplicated Ascites:
In this type, the fluids are not infected. This type is broken into three levels:
- Grade 1: Mild; an ultrasound is required to detect fluids
- Grade 2: Moderate; symmetrical distention and swelling of the abdomen occurs
- Grade 3: Severe; large or extreme distention of the abdomen occurs
Refractory Ascites:
When fluid buildup cannot be reduced by a low-sodium diet or diuretics, it is considered refractory, meaning that more aggressive treatment may be required.
Ascites can occur in children as well. It is most commonly associated with liver, kidney and heart disorders. The symptoms are similar to those found in adults, and treatment is similar.
Causes and Risk Factors
In the vast majority of patients diagnosed with ascites, 75 percent also have cirrhosis.
Often occurring in the gastrointestinal tract, other issues associated with this condition include:
- carcinoma of the stomach, colon or pancreas
- metastatic liver cancer
- hepatocellular carcinoma
- Meigs’ syndrome (carcinoma of the ovary)
- Hodgkin’s lymphoma and non-Hodgkin’s lymphoma
- metastatic carcinoma within the abdominal cavity
Of special note for malignancies is ovarian cancer. As the cancer spreads to the peritoneum, the first symptom experienced may be ascites.
Other rare causes include:
- Congestive heart failure: 3 percent
- Tuberculosis: 2 percent
- Pancreatitis: 1 percent
- Remaining rare causes: 4 percent
The remaining 4 percent of rare causes include:
- nephrotic syndrome
- hypothyroidism
- protein-losing enteropathy
- ovarian hyperstimulation from IVF procedures
- autoimmune inflammation of the liver
- inflammation of the pancreas or gallbladder
Cirrhosis is the most common cause. When the liver is damaged, blood flow through the liver is blocked. This causes an increased pressure on the main vein that is responsible for delivering blood from the digestive organs to the liver.
This is called portal hypertension.
Ascites then occurs as portal hypertension develops because the kidneys cannot get rid of enough sodium through urination. This causes fluids to build up in the abdomen.
Ascites is associated with a reduced rate of survival for those living with cirrhosis.
Ascites Risk Factors:
- Alcohol consumption
- Low-protein diet
- History of jaundice
- History of chronic hepatitis B or hepatitis C
- Obesity
- Hypercholesterolaemia
- Type 2 diabetes
- Nonalcoholic fatty liver disease
- Cardiac disease
- Certain types of cancer
- Kidney disease
Signs and Symptoms
Common symptoms of ascites include:
- Shortness of breath
- Rapid weight gain
- A feeling of fullness
- Large belly develops quickly
- Swelling in the ankles and legs
- Indigestion
- Vomiting
- Heartburn
- Loss of appetite
- Nausea
- Hernia
- Abdominal distention with mild to moderate discomfort
- Painful abdominal distention
- Jaundice
- Muscle wasting
- Fever
Conventional Treatment
Before treatment can begin, a proper diagnosis is required. If only small amounts of fluids are suspected, an ultrasound may be ordered.
Other tests may be required, including diagnostic tests for paracentesis as well as further ultrasounds to evaluate the liver, pancreas and lymph nodes. With these results, further testing may be required, including more specific imaging to look for signs of portal hypertension.
In addition, blood tests that measure liver function, electrolytes and a full blood count may be ordered. Once diagnosed, patients need to be screened for the development of spontaneous bacterial peritonitis, which occurs in some patients diagnosed with both ascites and cirrhosis of the liver.
Tests will search for the underlying cause of ascites. In addition to treating the cause, a salt-restricted diet is often employed as are diuretics.
Therapeutic paracentesis, a clinical procedure where a needle is inserted into the peritoneal cavity and fluid is removed, may provide temporary relief. The last treatment option, for the most advanced cases, is a liver transplant.
For children diagnosed with ascites, the condition is treated in much the same manner:
- Limiting sodium and liquids
- Prescribing diuretics
- Administering intravenous albumin
- Inserting shunts
- Prescribing antibiotics to prevent infection
- Liver transplantation
In children, specific complications are indicated with ascites and can include developmental delays, respiratory problems, fluid development and poor eating habits.
Natural Ways to Manage Symptoms
1. Restrict Salt
Salt restriction is associated with a lower diuretic requirement, faster resolution of ascites and shorter hospitalization for those with cirrhotic ascites, according to a randomized study from 1986 published in the journal Gut. Half of the participants were given a low-sodium diet of 21 mmol per day, and the other half was unrestricted on sodium intake. Both groups received diuretics.
While this is an older study, the American College of Gastroenterology states: “The most important step to treat ascites is to strictly reduce sodium intake,” placing salt restriction at the top of the list.
To this day, sodium restriction is a major part of treatment for ascites and part of the accepted guidelines on the management of ascites in cirrhosis.
Following a high blood pressure diet that focuses on eating fresh vegetables and fruit, lean proteins, legumes, healthy fats, sprouted whole grains, and organic dairy products, along with limiting any excess salt in the diet, may help relieve fluid retention.
2. Eat More, Smaller Meals
If appetite is low, which is common for those with ascites, try eating small meals four to seven times a day as recommended by the U.S. Department of Veterans Affairs. Some individuals may benefit by obtaining protein from plant sources, including nutritional yeast, ancient grains, vegetables, legumes and dairy products, instead of meat.
3. Avoid Toxins and Chemicals
Eat organic whenever possible because when the liver is damaged and not functioning optimally, it cannot properly detoxify and clear toxins from the blood. As it builds up, the toxins can move to the brain, causing a condition called hepatic encephalopathy.
4. Drink Coconut Water
High in potassium and other electrolytes, coconut water can help you stay properly hydrated even when on a liquid-restricted protocol. It’s been used as a diuretic to help treat saline-loaded rats in research, and it’s been shown to help suppress hepatic inflammation in an in vitro model of sepsis.
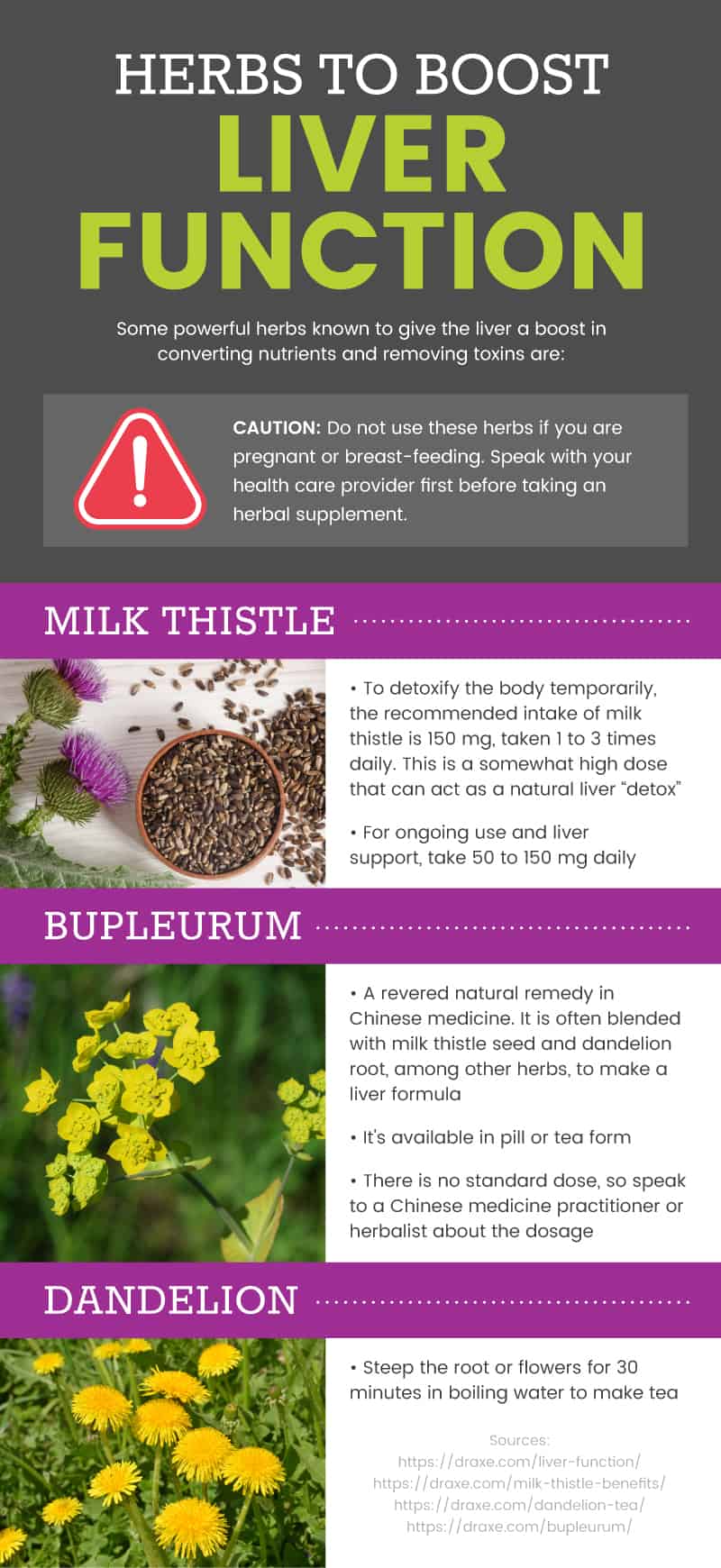
5. Drink Dandelion Root Tea
According to the results of a small pilot study conducted by the Tai Sophia Institute’s Department of Herbal Medicine, ingesting dandelion significantly increases urinary frequency and volume within five hours of the initial dose. The researchers encourage further studies to establish the efficacy and dosing for dandelion use as a diuretic.
Dandelion has also been found to provide protective effects for the liver.
Dandelion tea is packed with potassium and vitamins A, C and K, and it provides a healthy dose of minerals, including calcium, iron and magnesium. If you have dandelions growing in your yard — and you and your neighbors don’t use weed killers or pesticides — you can add fresh dandelion stems to salads or even to a pesto sauce.
6. Branched-Chain Amino Acids (BCAA)
BCAA supplementation promotes muscle protein synthesis and increases muscle growth for some individuals. These essential nutrients are typically obtained through the diet by consuming meat, dairy and legumes.
Research indicates that supplementation of BCAA may be effective for improving brain function related to liver disease, muscle wasting and other conditions related to ascites.
In addition, a case report from 2009 determined that BCAA supplements helped reduced ascites and increased the quality of life in a patient with cirrhosis.
If you prefer, you can boost your BCAA intake through diet. Eat more grass-fed beef, wild-caught Alaskan salmon, raw grass-fed cheese, quinoa, pumpkin seeds and a high-quality whey protein, which has the highest concentrations of leucine, one of the key BCAAs for muscle health.
Precautions
Ascites is the most common manifestation in cirrhotic patients and is associated with a reduced survival rate.
Spontaneous bacterial peritonitis (SBP) is an acute bacterial infection of the fluids in the abdominal cavity and is considered a serious complication of cirrhosis. It is associated with poor long-term prognosis and a high risk of mortality.
Septic shock is a serious concern and can occur in patients with alcoholic cirrhosis, heart failure, Budd-Chiari syndrome or as a complication of any disease that causes ascites.
Those with a stable cirrhosis diagnosis who suddenly develop ascites symptoms should be examined as soon as possible for hepatocellular carcinoma.
Individuals with cirrhosis should limit nonsteroidal anti-inflammatory drugs, including ibuprofen and others, as they may diminish blood flow and limit salt and water excretion.
Final Thoughts
- Ascites is a common complication of cirrhosis of the liver, with nearly 50 percent of all cirrhosis patients getting ascites within the first 10 years of diagnosis. It is considered a frequent complication of end-stage liver disease.
- Fluid develops in the abdominal cavity as a result of a poorly functioning liver caused by cirrhosis, malignancies, heart failure or other underlying health conditions.
- Ascites can occur in children, and it is most commonly associated with liver, kidney and heart disorders.
- Conventional treatment focuses on relieving excessive fluid buildup through diuretics and liquid-restricted diets. As it progresses, more invasive procedures may be required, including a liver transplant.