This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Vasculitis: Inflamed Blood Vessels + 4 Natural Treatments
July 8, 2017
Vasculitis is a group of inflammatory disorders that affect the blood vessels. Vasculitis can affect both small or large arteries. This includes major blood vessels like the aorta, as well as capillaries, medium-sized veins. Or it can include a combination of different sized blood vessels. In some cases, vasculitis causes only a portion of an artery to become inflamed, resulting in less serious symptoms. But in other cases a whole artery can become damaged and impaired, which leads to other complications.
Can vasculitis be cured? For some with vasculitis, the condition will go into remission following treatment. This means it’s no longer active but still remains in their system. Symptoms may come back at a later time due to a variety triggers that affect the person’s immune system. For others, vasculitis is chronic (long-term) and won’t respond well to treatment. Most people are able to manage their symptoms well. But everyone reacts to treatment a bit differently. No matter what type of treatment a patient needs, certain habits and lifestyle changes can help to reduce symptoms. These changes might include eating an anti-inflammatory diet, staying moderately active, reducing stress, getting enough rest and taking certain supplements.
What Is Vasculitis?
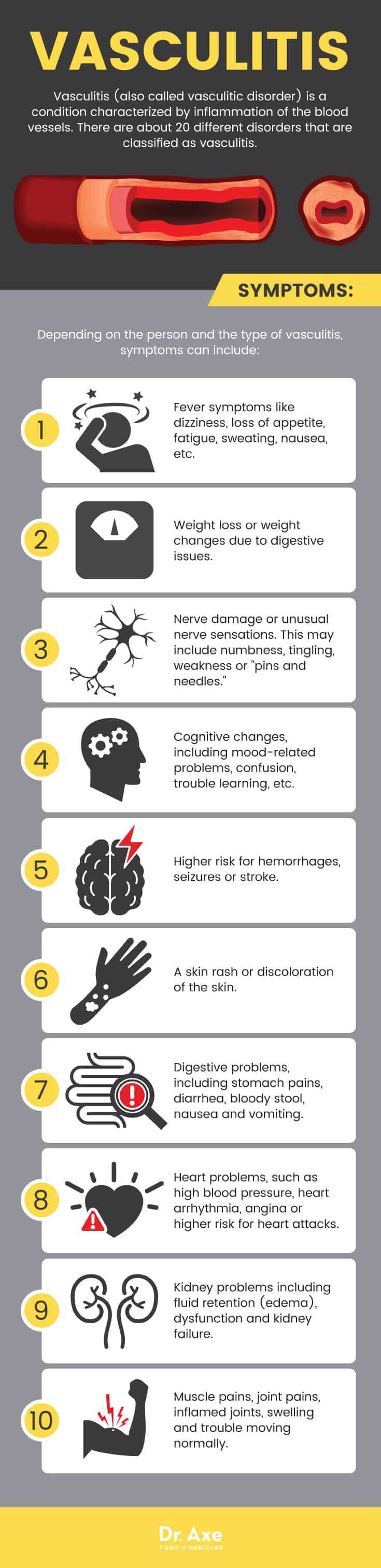
Vasculitis (also called vasculitic disorder) is a condition characterized by inflammation of the blood vessels, the series of tubular structures that carry blood to tissues and organs throughout the body. Vasculitis symptoms usually include fatigue, symptoms of a fever like nausea and weakness. Sometimes it causes more serious complications due to the vital organs not receiving enough blood. It’s not entirely known why some people develop vasculitis. But researchers believe that causes include acquiring certain viruses or infections, or a history of using certain drugs or medications. (1)
Various systems in the body can be negatively impacted by vasculitis, depending on which arteries are “attacked” by the immune system. For example, arteries that supply the vital organs with blood and nutrients can sometimes suffer. This can include arteries that fuel the brain or liver. Sometimes vasculitis affects several different organs or systems at once. But in other people only one organ (such as the skin) may become damaged.
Common Vasculitis Signs & Symptoms
Vasculitis symptoms will depend on which organs are affected most and how widespread the inflammation becomes. Sometimes vasculitis symptoms are directly due to inflammation of the arteries. But other times secondary/indirect symptoms develop due to ongoing damage of organs and destruction of tissue.
It’s common for vasculitis symptoms to be mild at first. Then they become worse as inflammation increases and the condition progresses. Because vasculitis symptoms are widespread and non-specific (they can be caused by many different health issues), it can be hard for patients to receive a proper diagnosis quickly. Each case of vasculitis is a bit different. Plus there are multiple types of vasculitis that cause different symptoms (more on this below). Depending on the person, vasculitis symptoms can include:
- Fever symptoms like dizziness, loss of appetite, fatigue, sweating, nausea, etc.
- Weight loss or weight changes due to digestive issues.
- Nerve damage or unusual nerve sensations. This may include numbness, tingling, weakness or “pins and needles.”
- Cognitive changes, including mood-related problems, confusion, trouble learning, etc.
- Higher risk for hemorrhages, seizures or stroke.
- A skin rash or discoloration of the skin. This may include the skin appearing bumpy, developing sores or ulcers (especially on the lower legs), or appearing dark due to hemorrhaging that results in bluish-red bumps.
- Digestive problems, including stomach pains, diarrhea, bloody stool, nausea and vomiting.
- Heart problems, such as high blood pressure, heart arrhythmia, angina or higher risk for heart attacks.
- Kidney problems including fluid retention (edema), dysfunction and kidney failure.
- Muscle pains, joint pains, inflamed joints, swelling and trouble moving normally.
- Coughing, shortness of breath, chest pains and trouble exercising due to difficulty breathing.
- Mouth sores or sores on the genitals.
- Ear infections.
- Headaches.
- Higher risk for blood clots.
- Problems with vision and developing painful, irritated eyes.
- In rare cases, life-threatening complications can develop that affect the heart, kidneys and lungs when a person does not respond to treatment.
- Some people also experience secondary mental health problems like fear, anxiety, depression and stress due to feeling overwhelmed by their condition. This can lead to decreased quality of life if it’s left untreated.
Types of Vasculitis
According to the Johns Hopkins Vasculitis Center, “There are approximately 20 different disorders that are classified as vasculitis.” (2)
There are a number of different names for subtypes of vasculitis depending on which parts of the body are affected. These include the conditions called: (3)
- Systematic vasculitis — When several different organs are affected due to multiple inflamed arteries. This usually causes widespread symptoms that affect the whole body.
- Cogan’s syndrome — Describes the type of vasculitis that affects large blood vessels, especially the aorta and aortic valve (the main artery that carries blood away from your heart to the rest of your body).
- Polyarteritis nodosa— When inflammation occurs in medium sized arteries throughout the body.
- Autoimmune inflammatory vasculitis — this is when someone has an existing autoimmune disorder that causes the immune system to attack the body’s own tissue (such as lupus, rheumatoid arthritis or scleroderma) and then develops vasculitis.
- Takayasu arteritis — When inflammation occurs in the aorta, vessels connecting the aorta and pulmonary arteries.
- Behcet’s disorder — Chronic inflammation that causes recurrent mouth sores.
- Churg-Strauss syndrome — Inflammation of the blood vessels in the lungs, sinuses and nasal passageways which commonly happens in people with asthma.
- Giant cell arteritis — Inflammation of the blood vessels in the upper body including the head, temporal lobes and neck.
- Henorch-Schonlein purpura — Inflammation of the blood vessels in the skin, kidneys and intestines.
- Microscopic polyangiitis — Inflammation of the small arteries in the lungs and kidneys.
- Wegener’s granulomatosis — Inflammation of the small arteries in the sinuses, nose, lungs and kidneys.
Vasculitis Causes and Risk Factors
Vasculitis is caused by inflammation and autoimmune reactions that attack the body’s own blood vessels. Like with other autoimmune disorders, such as Hashimoto’s thyroiditis or rheumatoid arthritis, the body mistakenly believes that a part of its own body (in this case the blood vessels) is foreign and therefore potentially a threat.
Inflammation occurs when cells of the immune system surround and infiltrate the blood vessels in order to damage them and try to weaken them. This can interfere with normal blood flow because the inflammation causes narrow, leaky, weak or clogged blood vessels, which can no longer carry oxygen and nutrients throughout the body. Tissues normally supplied blood by the affected/inflamed blood vessel will then become deprived of essential nutrients and therefore very damaged, sometimes even “dying off” due to permanent complications. (4)
People of all ages and ethnicities can develop vasculitis. However, there are certain risk factors that increase someone’s chances, especially having a history of dealing with serious infections or viruses like hepatitis C that fire-up the immune system. The following are risk factors for developing vasculitis:
- History of hepatitis B or C infection
- Having another autoimmune disease
- Recent infections
- Being a smoker or heavy drinker
- Having asthma
- Being between the ages of 15–40 increases risk for certain types of vasculitis including Behcet’s and Takayasu’s. However, being over the age of 50 increases risk for giant cell arteritis.
- Family history of vasculitis. Certain genes may contribute to vasculitis, particularly the gene called HLA-B51, which seems to play a role in Behçet’s disease. People who have a Mediterranean, Middle Eastern, or Far Eastern background may be at a higher risk for this type.
Conventional Treatment for Vasculitis
To make a diagnosis of vasculitis, your doctor will likely want to discuss your medical history, symptoms, family history and risk factors. Many people will receive a urine test, blood test and biopsy of an affected blood vessel to confirm the diagnosis and rule out other causes. The patient may also need X-rays, MRIs and other tests if the kidneys, brain, nerves or heart are believed to be impacted. The goal of treatment is to lower inflammation of the blood vessels in order to relieve symptoms by restoring normal or near-normal circulation. (5)
Once the doctor confirms that someone has vasculitis, conventional treatments will typically include:
- Use of medications to control inflammation — especially corticosteroids (like the kinds called prednisone, prednisolone and methylprednisolone) and other drugs that suppress the immune system (called immunosuppressants).
- Medications sometimes used when steroids don’t work include azathioprine, methotrexate, and cyclophosphamide.
- A variety of other drugs and medications might be used to control symptoms like skin rashes, high blood pressure, kidney dysfunction, etc. These can include antihistamines, skin ointments, diuretics, etc. To help decrease pain and swelling, patients can also use over-the-counter pain-killers, including acetaminophen, aspirin, ibuprofen or naproxen. While they are helpful for managing inflammation, it’s risky for patients to use corticosteroids long-term because they can cause complications like decreased bone density or osteoporosis, reduced immunity, electrolyte imbalances, bladder irritation and others.
- Recently, a newer treatment called rituximab has shown positive results for people with certain types of vasculitis. These include microscopic polyangitis and Wegener’s granulomatosis. Rituximab is a synthetic antibody that selectively reduces the number of B cells circulating in the blood. Because of this, it helps to decrease inflammation without the use of steroids. It also treats other autoimmune disorders, including B-cell lymphomas, chronic lymphocytic leukemia and rheumatoid arthritis. Because it can help eliminate the need for ongoing steroid use and help prolong remission, this new treatment is offering hope for many vasculitis patients. (6)

4 Natural Treatments for Vasculitis
1. Eat an Anti-Inflammatory Diet
Roughly 70 percent of your immune system is in your GALT. GALT means “gut-associated lymphoid tissue.” This is the reason why a healthy diet is so important for controlling inflammation and supplying your body with the fuel it needs. It’s recommended that people with vasculitis usually visit a dietitian, at least initially, to learn which types of specific dietary changes might be most helpful.
Every person will be different when it comes to the type of diet that will work best to manage flair-ups; however, almost everyone can benefit from eating anti-inflammatory foods that are minimally processed. To help keep inflammation levels as low as possible, the Vasculitis Foundation recommends following a healthy diet similar to one that is recommended by organizations like the American Heart Association. Here are several steps to take to control autoimmune reactions and decrease symptoms associated with leaky gut syndrome or deficiencies:
- Reduce or eliminate foods that may be hard to digest and contribute to gut trouble. These include gluten, excess sugar and conventional dairy products. You may want to do this for a period of time in order to track your symptoms and identify which foods are most problematic (in other words, follow an elimination diet).
- Avoid eating processed meats, raw seafood or undercooked meat. Eating these can increase the odds of negative reactions in people with suppressed immune systems.
- Reduce intake of caffeine, sweetened beverages and alcohol, which can worsen digestive problems.
- Try to stick to eating whole, unprocessed foods that are low in salt/sodium, especially if you have high blood pressure. Increase intake of electrolytes like potassium and magnesium by eating foods such as: leafy green veggies, other non-starchy veggies like broccoli or cabbage, bananas, avocado, sweet potato, almonds, yogurt/kefir, black beans, coconut water or milk and pumpkin seeds.
- If vasculitis has caused diabetes, kidney problems or renal insufficiency, then speak with your doctor or a dietician about specific restrictions in regards to your intake of carbohydrates/sugar, protein and foods that are high in potassium, because these can worsen kidney function and insulin production.
2. Supplement To Increase Immunity & Reduce Side Effects of Medications
While taking supplements or changing your diet won’t be enough to prevent or treat vasculitis, the supplements and herbal treatments below can help to strengthen the immune system and reduce the risk for complications. They may also help you cope with fatigue or stress and lower side effects due to taking corticosteroids or other medications (such as bone loss): (7)
- Calcium — According to the Vasculitis Foundation, “All patients treated with prednisone should be on supplemental calcium (1,000-1,200 mg daily) and vitamin D (800 IU daily) therapy unless contraindicated.” While calcium supplements might not be appropriate for the general public, they are needed by patients taking steroids long term due to how these drugs interfere with bone mineral density.
- Vitamin D — Many people are deficient in vitamin D, which takes a toll on the immune system, skeletal system and mental health.
- B vitamins — To help with reducing fatigue or brain fog, B vitamins can be helpful. Most multivitamins contain the daily recommended amount of B vitamins; however, it’s best to take a whole foods-based vitamin to ensure they’re absorbed well.
- Apple cider vinegar (ACV) — Some find that taking ACV helps to decrease digestive symptoms. It’s also beneficial for alkalizing the body and balancing the pH level within the digestive tract.
- Herbal remedies — These include anti-viral herbs or foods like raw garlic, turmeric, echinacea, calendula and adaptogen herbs like ashwaganda, holy basil and medicinal mushrooms. A variety of herbs contain anti-inflammatory, antiviral, antibacterial and astringent properties that support the immune system and lymphatic drainage. It may be a good idea to visit an herbalist or naturopath to discuss which types might be most helpful based on your symptoms.
3. Balance Activity With Rest
Even if your immune system is under a lot of stress due to dealing with your illness, you can still do most (or all) of the activities that you enjoy. Most people with vasculitis who are not dealing with severe symptoms can still work normal jobs and participate in recreational activities and even moderate exercise. Staying moderately active — such as walking, stretching and some gentle exercise like swimming or cycling — can help to manage certain symptoms like joint pain and depression. However, it’s important to pay attention to your own biofeedback because everyone is different.
While staying active and engaged is helpful, definitely also make it a priority to get enough rest and sleep. People who are overcoming autoimmune health problems and dealing with fatigue usually need eight or more hours of sleep each night.
4. Get Support From Family, Friends Or a Professional
If you’re feeling fearful or very stressed over your condition, it can be a good idea to speak with a professional counselor or therapist. This is especially important since stress can further weaken the immune system. Some people struggling with serious illnesses wind up feeling depressed and isolated. This can take a toll on a person’s well-being. It can make it even harder to overcome the condition. Try opening up to your family, friends and support network about your struggles. Or you may even want to find a support group online or in person. Consider asking your doctor to recommend a therapist who has experience working with people who are dealing with stressful health conditions.
Precautions Regarding Vasculitis Treatment
Your doctor will need to monitoring you to make sure that your vasculitis medications are not causing serious side effects. Relapses can also occur, which means the condition usually needs to be managed long term. No matter the course of treatment, it’s important to keep up with doctor’s appointments in order to check for secondary effects associated with the disease itself or medications. These can include osteoporosis, high blood pressure, high cholesterol, infections and development of certain types of cancers.
Final Thoughts on Vasculitis
- Vasculitis is a group of disorders that all have in common inflammation within blood vessels. There are at least 20 different types of vasculitis diseases that cause widespread symptoms affecting every system in the body.
- Causes of vasculitis are not entirely known. But they can include hepatitis or other viruses, infections, other autoimmune disorders or genetics.
- Treatments for vasculitis include medications like corticosteroids or immunosuppressants; an anti-inflammatory diet; rest; exercise; herbal remedies and supplements.