This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Hiatal Hernia Symptoms + 5 Natural Remedies
March 11, 2017
Different types of hernias develop inside different parts of the body, causing an abnormal bulging of one area into another. A hiatal hernia, also known as a hiatus hernia, forms inside the diaphragm, the muscular area that lays between the chest and the lower abdomen. It’s the most common diaphragmatic hernia, with the prevalence rate of hiatal hernia is between 13 percent to 60 percent of all adults. This includes roughly half of those over the age of 50. However, many people with a hiatal hernia have no idea because they never experience noticeable symptoms.
The abdomen holds most of the most important organs of the digestive system. These include the lower part of the esophagus, stomach, small intestine, colon, rectum, liver, gallbladder, pancreas, spleen, kidneys and bladder. When the abdomen experiences injury, lots of pressure, straining or inflammation, then any of these organs can dysfunction. Middle to older-aged women (over 50 years old) develop hiatal hernias more than any other group. The risk only goes up if the woman is overweight, obese, ill due to another disease or pregnant, according to the Cleveland Clinic. (1)
If you’ve talked to your doctor about symptoms of heartburn, anemia, acid reflux or GERD, he or she might have recommended that you should be checked for a hiatal hernia. All of these conditions are related and develop due to similar causes. These causes include eating a poor diet, being overweight/obese, taking certain medications, or high levels of inflammation.
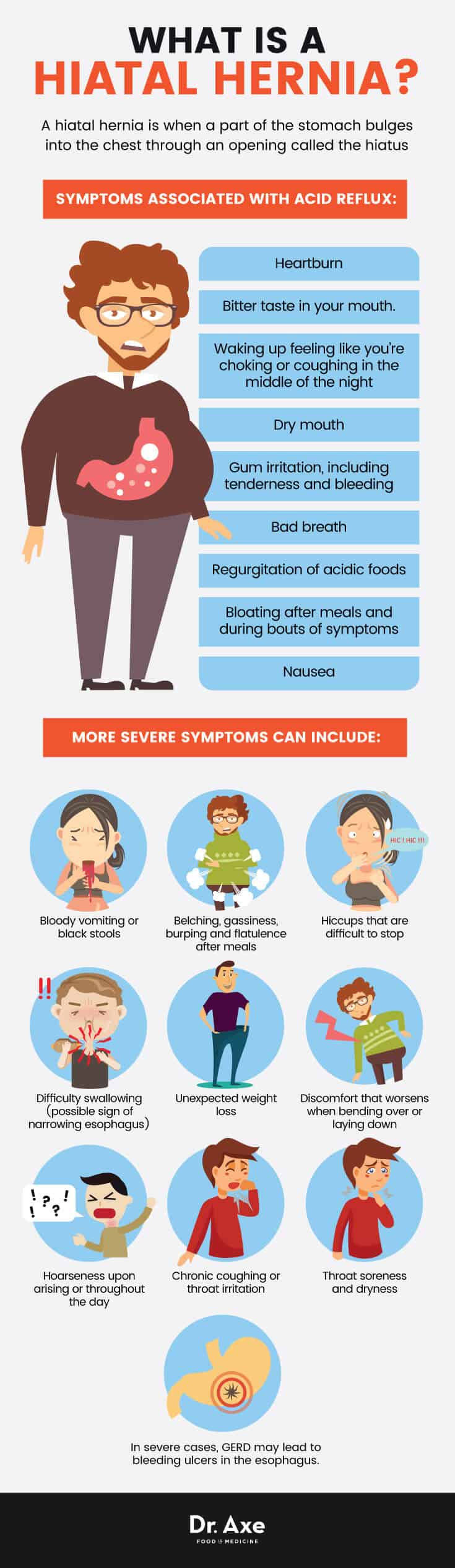
What Is a Hiatal Hernia?
A hiatal hernia is when a part of the stomach pushes into the chest through an opening called the hiatus. The hiatus is part of the digestive system that connects the stomach to the esophagus (also called the food pipe). (2) Officially, there are four types of hiatal hernias. Type I, the most common, occurs when “there is a widening of the muscular hiatal tunnel and circumferential laxity of the phrenoesophageal membrane, allowing a portion of the gastric cardia to herniate upward.” Types II, III and IV also involve the phrenoesophageal membrane and account for 5 percent to 15 percent of all hiatal hernias. (3)
Type II results from a defect in the phrenoesophageal membrane, type III have elements of both type I and type II, and type IV results from a large defect in the phrenoesophageal membrane.
While a hiatal hernia sounds like a pretty painful condition, given that the stomach pushes through an opening in the diaphragm and into the chest, most people with one don’t notice any symptoms.
When symptoms do occur, they include heartburn, acid reflux symptoms or developing a more severe digestive problem called gastroesophageal reflux disease (or GERD for short). Around 20 percent of all adults experience these symptoms on a regular basis, some almost daily.
While many people with hiatal hernia suffer from symptoms of heartburn/acid reflux, the hernia doesn’t seem to directly cause these conditions. Instead, whatever factors contribute to acid reflux (poor diet, inflammation, etc.) also contribute to hernias. Having a hiatal hernia isn’t a guarantee of developing acid reflux or GERD. However, some people have one condition without having the other, but research shows there is often overlap between the two. Additionally, hiatal hernia is common among those with Crohn’s disease.
Common Symptoms of a Hiatal Hernia
If someone does develop signs or symptoms of a hiatal hernia, usually they include chest pain, burning sensations and irritation of the throat. Other symptoms related to acid reflux, heartburn and GERD are also possible.
Symptoms associated with acid reflux include:
- Heartburn
- Bitter taste in your mouth. Periodically, or, for some people, throughout the day — some people taste regurgitated food or sour liquid at the back of their mouths/throats
- Waking up feeling like you’re choking or coughing in the middle of the night
- Dry mouth
- Gum irritation, including tenderness and bleeding
- Bad breath
- Regurgitation of acidic foods
- Bloating after meals and during bouts of symptoms
- Nausea
More severe symptoms can include:
- Bloody vomiting (possible sign of damage in lining of esophagus) or black stools
- Belching, gassiness, burping and flatulence after meals
- Hiccups that are difficult to stop
- Difficulty swallowing (possible sign of narrowing esophagus)
- Unexpected weight loss
- Discomfort that worsens when bending over or laying down
- Hoarseness upon arising or throughout the day
- Chronic coughing or throat irritation
- Throat soreness and dryness
- In severe cases, GERD may lead to bleeding ulcers in the esophagus. It also can lead to a dangerous condition called Barrett’s esophagus, which can lead to esophageal cancer.
Types of Hernias
There are several different types of hiatal hernias. Two are the most common: sliding (the most common type and also the one associated with development of GERD) and paraesophageal. These are also called type I and type II, while type III is a combination of both.
- Sliding hiatal hernia (type 1, also called concentric or axial hiatal hernia, or sliding hiatus hernia): Sliding hiatal hernias account for more than 95 percent of all hiatal hernias. This type occurs when the stomach moves into the opening leading to the chest through the hiatus, resulting in a sliding hiatus hernia. Normally, the gastroesophageal junction keeps stomach acid inside the stomach (it has an “antireflux barrier function”). This is compromised in patients with hiatal hernia. Stomach acid leaks out of the stomach and into the lower esophagus, causing GERD to develop. GERD may lead to reflux esophagitis, Barrett’s esophagus and esophageal adenocarcinoma. The doctor can use X-rays to diagnose hiatal hernias.
- Paraesophageal hiatal hernia (type 2): The remaining 5 percent of hiatal hernias are paraesophageal. This type develops next to the esophagus. Of the two types, paraesophageal hernia is riskier because it can lead to reduced blood flow reaching the stomach, contributing to complications like cell death and tissue damage.
- Type III hiatal hernia: This type is a mixture of type I and II hiatal hernia because it involves both defects.
- Type IV hiatal hernia: Caused due to herniation of other abdominal organs (spleen, colon, pancreas, etc.) through the esophageal hiatus.
Hiatal Hernia Causes and Risk Factors
Hiatal hernias occur when muscles surrounding the hiatus opening (which separates the esophagus from the stomach) become weak and stop functioning properly.
The esophageal hiatus is an oval-shaped opening that is controlled by certain ligaments and membranes. These ligaments and membranes are essential in maintaining control of the tissue of the stomach and also stomach contents (including acid). They normally work by sealing off potential spaces between the esophageal hiatus and the esophagus. They open and close depending on if you’ve just eaten something. (4)
When the swallowing muscles and tissues in the esophagus become inelastic, weak, strained or are exposed to too much stress and pressure, stomach acid and parts of the stomach can make their way into the lower esophagus (food pipe). This is why hiatal hernia is associated with heartburn, acid reflux and GERD.
Risk factors associated with hiatal hernias include:
- High levels of inflammation, which is linked to poor gut health.
- Eating a poor diet.
- Obesity or being overweight. This usually causes increased pressure in the abdomen. Since obesity is usually tied to eating a highly processed, poor diet it, can also contribute to inflammation and other forms of indigestion.
- Pregnancy, which puts pressure on the digestive organs.
- Chronic or strong coughing. This can be due to a respiratory illness such as an infection.
- Constipation (straining or pushing during bowel movements).
- Genetic factors. Some people are born with a larger-than-normal hiatal opening in their diaphragm, which increases the risk for hernia.
- Vomiting to the point of pushing too hard on the digestive muscles.
- Lifting heavy objects to the point of straining a muscle in the digestive tract.
- Injury to the diaphragm or abdomen.
- Older age, which is associated with muscle weakness.
- Recovering from surgery of the abdomen.
Complications Due to Hernias
1. Heartburn, Acid Reflux and GERD
For decades researchers believed that GERD and hiatal hernias were practically the same thing. Sliding hernias are most closely associated with acid reflux and GERD.
New insights show that acid reflux/GERD are tied to the same factors that cause hiatal hernia; however, they aren’t the same thing. Factors that contribute to both conditions include: abnormal esophageal acid clearance, tissue resistance, abnormal gastric acid secretion, delayed gastric emptying, and other functional abnormalities of the lower esophageal sphincter (LES). The relation between GERD and hiatal hernia is now referred to as the “two-sphincter hypothesis.” (5, 6)
Over time, if left untreated, GERD can sometimes lead to serious problems like reflux esophagitis, Barrett’s esophagus and esophageal adenocarcinoma (cancer of the esophagus). (7) Because of these risks, experts feel that it’s very important for doctors to investigate if a patient with occasional acid reflux symptoms also has a hiatal hernia and is more likely to experience GERD. The treatment of a hiatal hernia is similar to the management of GERD; lifestyle and dietary changes that help resolve one will also lower incidence and risk for the other.
2. Stomach Bleeding or Ulcerations
Surgery might be needed to control complications like stomach bleeding, ulcerations or strictures. These complications are most likely to occur when lots of pressure is placed on the abdomen and digestive organs. Intra-abdominal pressures can be due to chronic or strong coughing, abdominal straining and abdominal compression due to injury, and for other reasons that strain the tissues and organs.
Conventional Treatments for a Hiatal Hernia
Not every person who has a hiatal hernia needs treatment, especially since most don’t experience symptoms or pain. If you do have symptoms, your doctor can diagnose a hiatal hernia by performing an endoscopy test, a pH test, barium swallow scans or X-rays to look for abnormalities inside the esophagus. Once the doctor finds a hiatal hernia, treatments will depend on how severe your symptoms are, if there are any complications that have developed, and how often you deal with pain due to heartburn/acid reflux/GERD. Most of the time treatments are used to control GERD symptoms.
- Antacids, H2 blockers or use of other medications. These are commonly used to manage symptoms of heartburn/acid reflux. Some lower acid production while others block acid’s effects, or help clear stomach acids quicker. Medications can include over-the-counter antacids, H2 blockers, proton pump inhibitors (PPIs), and prokinetics for other stronger prescriptions.
- Lifestyle changes. Try improving your diet, losing weight, being more active, managing stress, changing medications if needed, and changing your sleep position. More on these natural remedies is covered below.
- In severe cases, hernia surgery. Surgery is sometimes needed if part of the stomach moves into the hiatus, which cuts off blood flow to the stomach. Laparoscopic surgery is one of the common surgical methods used for fixing hernias. The surgeon only makes small incisions to perform laparoscopic surgery using a laparoscope. The risk is believed to be relatively low for lots of scarring or complications during recovery. This type of operation can include fixing or removing the hernia sac, tucking the stomach back in its correct place and out from the esophagus, making the opening of the hiatus smaller, or reconstructing a weak esophageal sphincter. (8)
- Manipulation of the Stomach. Some choose to see alternative practitioners who manipulate the stomach non-invasively by hand to push it back to its correct position. There isn’t strong evidence that this works for everyone.

5 Natural Remedies for a Hiatal Hernia
1. Treat Acid Reflux/Heartburn Symptoms With A Healthy Diet
A poor diet can contribute to an overactive immune system, which causes all sorts of painful symptoms. Here are foods that tend to make acid reflux or GERD symptoms worse for many people. Cut down on these if you’ve been diagnosed with a hiatal hernia:
- Alcohol
- Too much caffeine
- Carbonated beverages, sugary drinks or energy drinks
- Artificial sweeteners
- Fried, greasy or very fatty foods
- Refined vegetable oils, including canola oil
- Spicy foods
- Chocolate and cocoa
- Citrus fruits, garlic, onions and tomatoes
- Processed foods and those very high in sodium or synthetic additives
There are also healthy foods that can help improve these symptoms. Include plenty of these in your diet: (9)
- Fresh organic vegetables (especially leafy greens, squash, artichoke, asparagus and cucumbers)
- Probiotic foods like yogurt or kefir
- Fruits (if you can tolerate them well) like berries and melon
- Lean proteins like free-range chicken and wild-fish
- Bone broth
- Healthy fats like coconut or olive oil
- Herbs like parsley, ginger, and fennel.
- Apple cider vinegar
- Aloe vera gel
2. Maintain a Healthy Weight
Being overweight or obese puts extra pressure on the valves and sphincter that allow release of stomach acid. In addition, obesity is often associated with low levels of stomach acid. (10) In eight of nine studies included in a large review, as BMI (body mass index, a measure of body fat ) rose, so did GERD symptoms. Try to reach and remain at a healthy weight. Eat an unprocessed diet, get more exercise and manage other unhealthy habits.
3. Change Your Sleep Position
Try not to head to bed for several hours after eating dinner, since lying down can make symptoms worse. Relax after your last meal of the day, stay upright for 3 hours and try to avoid being completely stationary. For help with controlling flow of stomach contents, adjust your sleeping position. Sleep on a slight angle and raise the head of your bed 6 to 8 inches. You can do this by using a bigger pillow by placing lifters or blocks under your bedposts. Struggle to get good sleep many nights in general? Try exercising more during the day. Exercise may help you fall asleep more soundly and also has many benefits for digestive health including lowering inflammation.
4. Quit Smoking
Smoking cigarettes increases inflammation and impairs muscle reflexes that are important for controlling release of digestive contents. Smoking may also increase production of stomach acid. Avoid smoking if you are suffering from acid reflux.
5. Eat Mindfully & Manage Stress
High levels of stress can have devastating effects on digestion for some people. Stress can raise inflammation levels and alter gut health. It can also contribute to unhealthy habits like over-eating, eating lots of processed foods, eating too quickly, not getting enough rest, not exercising and skipping meals. You can help slow down symptoms of indigestion. Eat smaller meals rather than large meals only 1-3 times per day. Eat more slowly, chew your food well and relax (in other words eat mindfully). Work on managing stressors in your life through practices like meditation, reading, exercise, spending time outdoors, etc.
Precautions When Treating Hiatal Hernias
The most important warning signs associated with a severe hiatal hernia risk include: severe pain in the chest or abdomen (some say this feels “like having a heart attack”), sudden nausea and vomiting, lots of trouble breathing normally, feeling like you’re choking or wheezing, sudden and severe hoarseness in your voice, and severe constipation or painful bloating/gas. Talk to your doctor right away, or seek emergency care.
Final Thoughts on Hiatal Hernias
- A hiatal hernia, aka hiatus hernia, happens when a part of the stomach bulges into the chest through an opening called the hiatus, which connects the stomach to the esophagus (food pipe).
- Symptoms of a hiatal hernia include those associated with heartburn, acid reflux or GERD. These can include chest pains, burning sensations, sour taste in your mouth, loss of appetite and other forms of indigestion.
- Causes of hiatal hernias are muscle weakness in the abdomen, straining the digestive tissues and high levels of inflammation. Risk factors are eating a poor diet, obesity, older age, stress, genetics, injury to the abdomen and pregnancy.
- Natural remedies include reducing inflammation, changing your diet, losing weight, quitting smoking and altering your sleep position.


