This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Brain Zaps + 4 Brain Zaps Natural Remedies
October 31, 2018

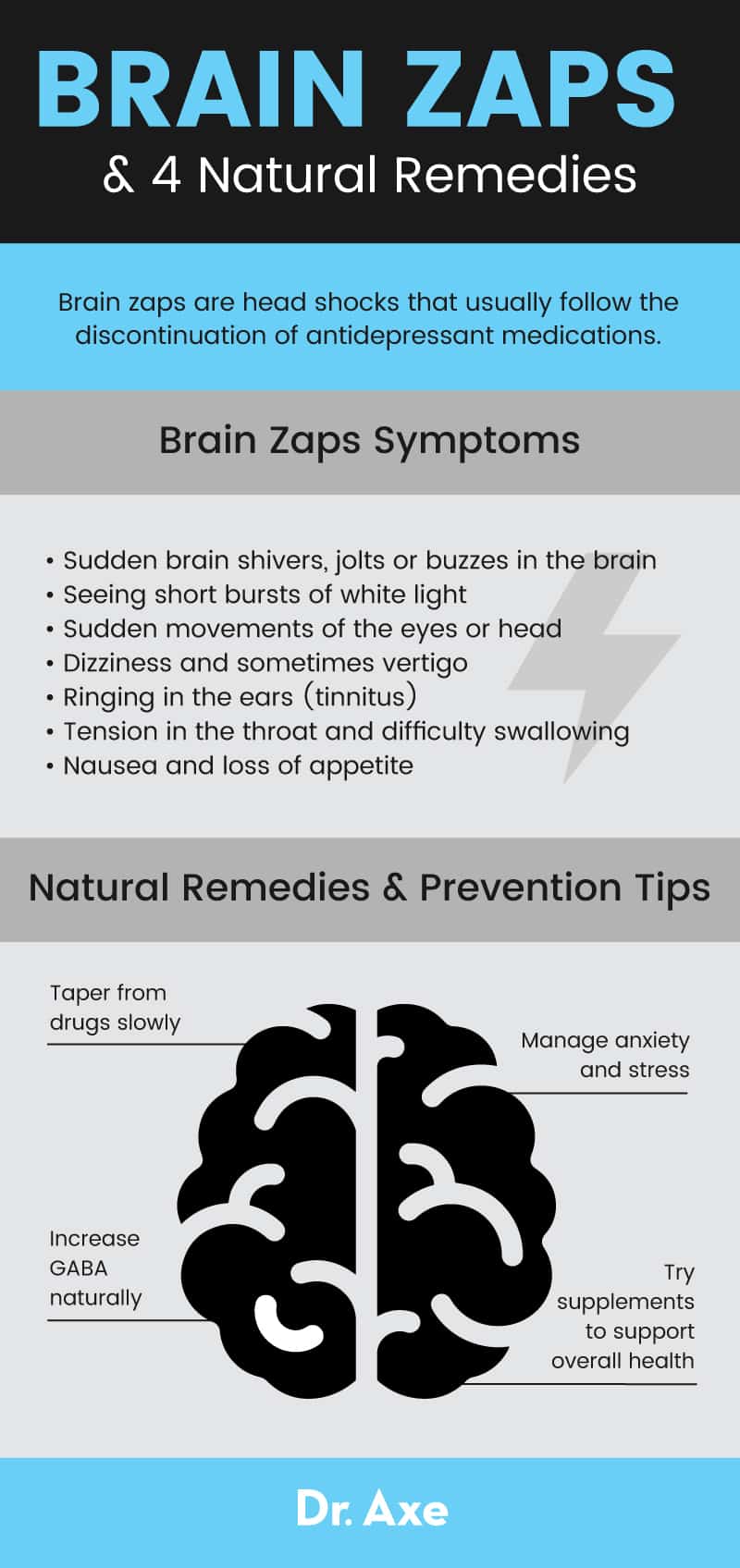
Brain zaps — also sometimes referred to as brain shivers, brain shocks or head shocks — are described as being one of the most unbearable withdrawal symptoms when stopping certain depression and anxiety medications. Brain zaps get their name from the uncomfortable sensations they cause that are described as feeling like sudden zaps, electrical buzzes, tremors, shakes or jolts in the brain.
According to a New York Times analysis, the fear of dealing with withdrawal effects like brain zaps is believed to keep millions of people on antidepressant medications every year, even when they think they can cope well without them. (1) For example, a 2017 survey of 250 people who were considered long-term users of psychiatric drugs (mostly antidepressants) found that nearly half of users experienced severe antidepressant withdrawal symptoms when attempting to discontinue use of their drug. Half also reported they could not/would not stop taking the drug because of potential withdrawal symptoms. (2)
Can brain zaps be prevented and/or treated? Currently there is no medical intervention or medication that can be used to reliably control brain zaps. However, natural remedies have helped many people avoid serious antidepressant withdrawal symptoms, including: tapering off from drugs slowly, managing stress/anxiety, increasing GABA naturally and taking supplements that support cognitive health.
What Are Brain Zaps?
Brain zaps are head shocks that usually follow the discontinuation of antidepressant medications — which is why they are typically considered a withdrawal effect and associated with “antidepressant discontinuation syndrome.”
What Do Brain Zaps Feel Like?
Most people who have suffered from brain zaps say they come out of nowhere, usually last only a few brief moments and then disappear. There doesn’t seem to be clear triggers or any warnings that one is coming. Some people find that they deal with brain zaps when falling asleep or shortly after waking up from sleep. Brain zaps might also be triggered by alcohol use, anxiety or stress.
Brain zaps can cause some of the following symptoms and sensations: (3)
- Sudden brain shivers, jolts or buzzes in the brain. Some people feel like their whole head is affected, while others say only a small part of their brain feels like it’s involved. Sometimes brain zaps may also feel like blood rushing to the head.
- Seeing short bursts of white light
- Sudden movements of the eyes or head
- Dizziness and sometimes vertigo
- Ringing in the ears (tinnitus)
- Tension in the throat and difficulty swallowing
- Nausea and loss of appetite
What Causes Brain Zaps?
What are the electric shock sensations known as brain zaps caused by? It’s not entirely known what causes brain zaps, but brain zaps are often associated with withdrawal from certain drugs, especially SSRIs, or selective serotonin reuptake inhibitors, the most commonly prescribed antidepressants for depression and anxiety.
What is discontinuation syndrome? It’s a temporary condition that can occur following the interruption, reduction or discontinuation of antidepressant medications. Examples of SSRIs that can cause discontinuation syndrome include: Sertraline (Zoloft), Citalopram (Celexa), Escitalopram (Lexapro), Fluoxetine (Prozac) and Paroxetine (Paxil, Pexeva).
Across the internet, many people have reported a connection between brain zaps and Zoloft withdrawal. Brain zaps are not the only withdrawal symptom that people weaning from drugs like Zoloft or Prozac can experience — other common withdrawal effects include dizziness, headaches, nausea and paresthesia (burning or prickling sensation that is usually felt in the hands, arms, legs or feet). And this does not even include antidepressant side effects that can occur while taking these medications, which often include: weight gain, fatigue, sleep disturbances, cognitive impairment, headaches, sexual dysfunction, constipation and sometimes suicidal thoughts.
Aside from SSRIs, brain zaps have been reported when discontinuing other drugs too, such as:
- Similar drugs to SSRIs called selective serotonin and norepinephrine reuptake inhibitors, or SSNRIs
- Benzodiazepines, prescribed for anxiety and to promote relaxation
- ADHD medications including Adderall (amphetamine salts)
- MDMA (or ecstasy), an illegal street/party drug
There have not been many studies conducted that have investigated why brain zaps occur, although one theory is that they are due to changes in levels of serotonin in the brain. SSRI and SSNRI medications work by blocking a serotonin transporter and increasing serotonin levels. They also increase GABA activity, one of the brain’s main “calming” chemicals. However, falling levels of serotonin are not believed to be the primary cause of brain zaps because it’s been found that people with low serotonin prior to taking these medications do not experience brain zaps. (4)
A current hypothesis for the cause of brain zaps is that they may be due to declining levels of GABA. Drugs associated with brain zaps (SSRIs, benzodiazepines, ecstacy and Adderall) are all associated with an increase in GABA levels in the brain, and we know from a number of studies that when GABA levels fall, a number of withdrawal symptoms are possible. For example, low levels of GABA can trigger seizures, so it’s been speculated that brain zaps may actually be a form of a mild, localized seizure.
4 Natural Treatments for Brain Zaps and Prevention
1. Taper From Drugs Slowly
At this time, more research is needed regarding the most effective antidepressant withdrawal treatments. One thing that may be able to limit symptoms like brain zaps is slowly tapering off drugs, rather than stopping cold turkey — especially if you have been taking a high dose or using the drug for a long duration of time. (5)
You might be able to decrease your chances of experiencing brain zaps when you stop your medication slowly; however, this strategy is not guaranteed to work. Unfortunately, studies have found that even when someone slowly tapers from a drug, many of the drugs have relatively long half-lives and can still cause significant withdrawal symptoms. This leads many people to restart the drug and to stay stuck in a vicious cycle.
2. Manage Anxiety and Stress
Although you might experience brain zaps for no obvious reason, they seem to be more common among people who are under a lot of stress or dealing with anxiety. Some people report that the intensity, duration and frequency of their brain zaps gets worse when they are dealing with elevated stress.
If stress remains elevated and becomes chronic, it’s not uncommon to experience brain zaps and other symptoms for years. An important part of your brain zap treatment plan should be managing stress and giving your body time to recover from any traumatic or exhausting events you’ve dealt with lately. If you suffer from depression or an anxiety disorder, it’s best to work with a trained counselor, coach or therapist who can help you learn how to manage your symptoms long-term.
Other stress-relieving activities that can be helpful include: yoga, exercise, meditation, time spent in nature, prayer, joining a faith-based organization/community, reading and journaling.
3. Increase GABA Naturally
Because GABA (gamma-aminobutyric acid) is a neurotransmitter that can help curb nervousness, anxiety and insomnia, it makes sense that by boosting levels naturally, you may lower your odds of experiencing brain zaps due to stress. GABA appears to have additional benefits too, such as helping to fight inflammation, PMS, weight gain, muscle loss, heart disease and ADHD. Many of GABA’s positive mood-enhancing effects are due to how it reduces/inhibits activity of certain nerve cells in the central nervous system.
Although we still need more research to confirm that declining GABA levels contribute to antidepressant withdrawal symptoms, there’s no downside in making the following types of lifestyle changes that support higher GABA production:
- Get quality sleep. Stick to a regular sleep-wake cycle, limit caffeine and alcohol intake and establish a calming “bedtime routine” to help you unwind at night.
- Eat a nutrient-dense, anti-depression diet that includes plenty of antioxidants, vitamins, minerals, amino acids and essential fatty acids from foods like fresh veggies such as leafy greens, fruits including berries, grass-fed meat, pastured eggs, wild-caught fish like salmon, probiotic foods and healthy fats like olive oil, coconut oil, walnuts, almonds, flaxseeds and other nuts/seeds.
- Get regular exercise, including high intensity (HIIT) workouts if possible.
- Quit smoking, drinking alcohol in excess (more than one drink per day on average) and using street/illegal drugs.
- Get sun exposure/spend time in nature to boost vitamin D levels.
GABA can also be taken in supplement form, typically in doses of about 250–650 milligrams, two to three times daily; however, supplementing with GABA is not safe for everyone, including pregnant or breast-feeding women or those taking a number of mood-altering medications.
4. Try Supplements to Support Your Overall Health
Supplements are not a quick-fix solution to getting rid of brain zaps or tackling anxiety and depression; however, some people do find that taking certain supplements helps to minimize withdrawal side effects and makes them feel better in general. Supplements that can be supportive of mental/cognitive health include:
- Omega-3 fatty acids (or fish oil supplements), which have anti-inflammatory effects
- Vitamin B12 and vitamin B6, which can support GABA production and fight symptoms like fatigue, weakness and brain-fog
- Vitamin D3, which is best obtained from exposure to sunlight but can also be taken in supplement form to prevent vitamin D deficiency
- Magnesium, which is helpful for sleep and fighting restlessness, muscle tension and symptoms associated with stress
- St. John’s Wort
- L-glutamine and L-arginine, which work with GABA to support growth hormone levels
- Valerian root, ashwagandha and rhodiola, all herbs which are naturally calming and beneficial for the nervous system
- Calming essential oils, such as lavender, ylang ylang and chamomile oil
One thing to point out is that it’s important to discuss supplements with your doctor if you’re currently taking medications, since interactions may occur.
Brain Zaps Precautions
Given that withdrawal treatment research still has a long way to go, when it comes to managing brain zaps, prevention is key. Talk to your doctor about alternatives to taking antidepressant medications. If you do choose to use drugs such as SSRIs, consider the duration of treatment you actually need. Keep in mind that antidepressant drugs like SSRIs were originally intended to be taken for about three to nine months — not years on end.
If you are on a particular drug for a long period of time, you will be more likely to experience brain zaps and other effects when stopping. You can also discuss the option of taking a drug that has a longer half-life with your doctor, since some stay in your system longer than others, which may help prevent withdrawal as levels gradually decline. No matter what, don’t stop taking any prescribed medication without getting consent from your doctor. If you’re going through a stressful period, make sure to work with a professional and don’t self-treat your condition by altering the amount/type of medication you take.
Final Thoughts
- Brain zaps are head shocks, or electrical-like sensations, that usually follow the discontinuation of medications such as SSRIs, benzodiazepines or ADHD medications.
- Brain zaps can occur along with other withdrawal symptoms like dizziness, nausea, loss of appetite, vertigo, numbness, headaches and ringing in the ears.
- There is no established brain zaps treatment that has been shown to work for everyone, since research is generally lacking when it comes to antidepressant drug withdrawal management.
- Natural remedies that may help you avoid serious withdrawal symptoms, such as brain zaps, nausea and dizziness, include: tapering off from drugs slowly, managing stress/anxiety, increasing GABA naturally and taking supplements that support cognitive health.



