This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
More Than 20 Natural Ways to Ease Esophagitis Symptoms
December 10, 2017
Esophagitis is inflammation of the esophagus (the muscular tube connecting your mouth to your stomach). It causes pain or difficulty swallowing food and pills, and can make eating very uncomfortable. When it goes untreated, esophagitis can lead to changes in the esophagus that can make it hard to swallow food without choking. (1)
There are many potential causes of esophagitis. Its symptoms can range from vomiting to chest pain, which are involved in many other health problems, so you shouldn’t try to self-diagnose esophagitis. By getting a formal diagnosis, you can get the right type of treatment. In most cases, esophagitis gets better with treatment. (2)
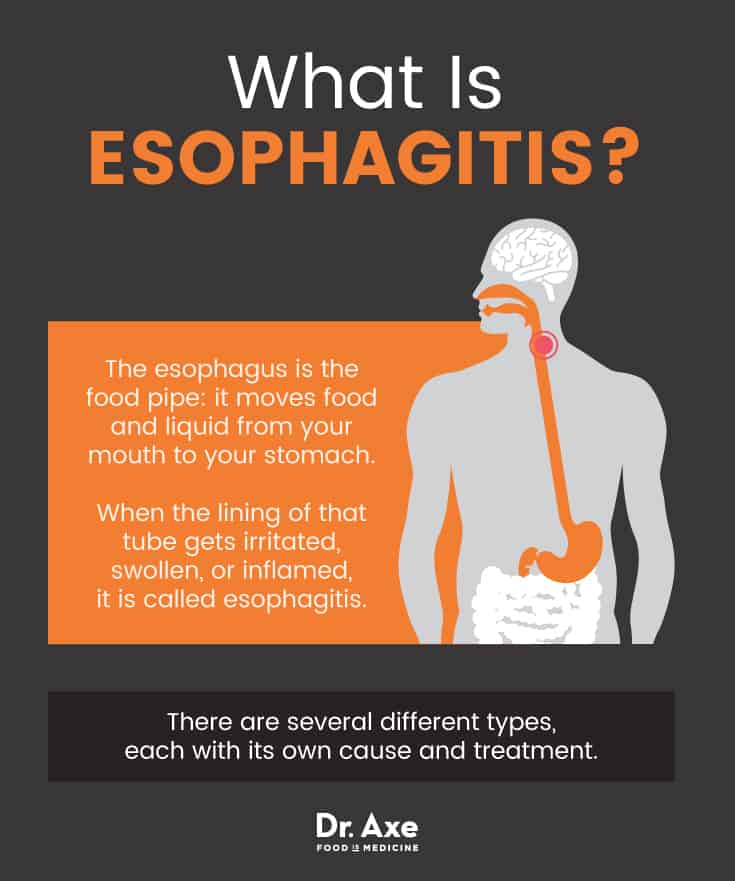
What Is Esophagitis?
The esophagus is the food pipe: it moves food and liquid from your mouth to your stomach. When the lining of that tube gets irritated, swollen, or inflamed, it is called esophagitis. (3) There are several different types, each with its own cause and treatment. Although rare, sometimes another condition known as achalasia may also occur with esophagitis. (4) Achalasia causes difficulty swallowing due to nerve damage in the esophagus. (5)
Types of esophagitis
- Reflux esophagitis: The bottom of the esophagus has a small valve (the lower esophageal sphincter) that helps keep stomach acid from coming back into the food pipe. If that opens when it shouldn’t, or if it doesn’t close correctly, stomach acid can get into the food pipe. This causes heartburn and irritation of the esophagus and is known as gastroesophageal reflux disease (GERD). When it lasts for a long time, GERD can damage tissue in the esophagus and cause swelling that is known as reflux esophagitis. (6)
- Eosinophilic esophagitis: In some people, white blood cells collect in the esophagus. These cells are called eosinophils. They are often an indicator of a food allergy or acid reflux (or both). (7) When these white blood cells are present in high amounts in the esophagus, it is called eosinophilic esophagitis. People with allergies to pollen, milk, eggs, wheat, nuts, beans, soy, rye and beef may not even know they even have an allergy causing the problem. (8) Skin tests for these allergens may be negative, and even blood tests may show very low-level allergic results. (9)
- Drug-induced esophagitis: This is also called pill-induced or medication-induced esophagitis. It is irritation or injury of the esophagus caused by taking pills without enough water. The pills can physically harm the esophagus, or they may leave behind some residue that stays in the food pipe and hurts the tissue. (10) In most cases, this type goes away after the medication is stopped, or with changes in how you take the medicine. (11) It can often be healed and avoided by taking pills while sitting or standing upright, with a full glass of water. (12)
- Infectious esophagitis: Infections can affect the tissue of the esophagus, causing esophagitis. The infections can be fungal, viral or bacterial. They occur most often in people with lowered immunity, such as people taking steroids or antibiotics, or people with diabetes, cancer or HIV/AIDS. (13) Otherwise, this type of esophagitis is fairly rare. When it does occur, it is often caused by Candida. (14)
- Lymphocytic esophagitis: This occurs when there is a high number of lymphocytes (white blood cells that help fight invaders such as bacteria or toxins) in the esophagus. (15) It is rare but related to eosinophilic esophagitis and GERD.
- Erosive esophagitis: Any type of esophagitis can become erosive if it begins to wear away the lining of the esophagus. Chronic acid reflux is the most common cause of erosive esophagitis, but drinking corrosive liquids (such as cleaning solutions), taking certain pills or having certain types of large pills get caught in the esophagus can all cause painful erosions. (16) These are also called lesions.
How is esophagitis diagnosed?
Although your doctor may have a good idea of an esophagitis diagnosis based on your symptoms, you are likely to have at least one test to confirm. You can expect to be diagnosed using one of these tests:
- Esophageal manometry: This checks how well your esophagus works and whether the lower esophageal sphincter (the valve leading to the stomach) opens and closes the way it should. (17) A tiny tube goes through your nose and down through your food pipe into the stomach. Then you rest on your side and swallow a sip of water. The tube is sensitive to pressure and measures how strong your muscles are and how well they work. (18)
- Esophagogastroduodenoscopy (EGD): This is a biopsy of your esophagus. They put you under light anesthesia and insert a small tube down your throat through your mouth. There is a camera on the end so that the doctor can see what your esophagus looks like. In most cases, they will take a piece of tissue from your esophagus, which is called a biopsy. (19)
- Lab tests: If you have a biopsy done, the tissue sample will be sent to a lab to check for things such as infection, white blood cells, or esophageal cancer or precancerous cells. (20)
- Esophageal X-ray: This is also called an upper GI series or barium X-ray. You will swallow barium (as a liquid or pill) and they will take X-ray images of your neck, chest and stomach to check the esophagus for damage or to search for other esophagus problems, like hernia or tumors. (21)
What is Grade 1 esophagitis? Grade IV? Esophagitis Grade A?
There are several scales that exist to measure how severe your disease is. The scales are often used in clinical research or by doctors to help decide how to treat your esophagitis or to track your improvement. Ask your doctor which scale they used to score you and what your grade level means.
In most cases, Grade 1, Grade I or Grade A mean there are minor signs of esophagitis, such as spots showing irritation or damaged tissue. With each step up in grade level (up to 4 or 5, or up to the letter D), the condition is considered more severe. The most severe stages involve damage to large percentages of the esophageal tissue. They usually also mean that there have been changes to the esophagus, called strictures, that make it narrower in certain places. Esophageal strictures or rings can make it very hard to swallow food. (22)
Esophagitis Signs & Symptoms
Esophagitis symptoms can be confused with symptoms of many other health problems, such as esophageal spasm or even a heart attack. (23) When symptoms alarm you, last more than a few days, don’t improve with over-the-counter heartburn or reflux medicines, or make it difficult for you to eat, see a doctor. (24) You should also get medical care if you have esophagitis symptoms together with headache, fever and muscle aches.
Symptoms of esophagitis include: (25, 26, 27)
- Trouble swallowing (also called dysphagia)
- Painful swallowing
- Chest pain during and after eating
- Food that gets stuck in the esophagus
- Heartburn
- Acid reflux
- Nausea or vomiting
- Coughing
- Sore throat
- Hoarse voice
In infants and young children, signs may include vomiting, trouble feeding and failure to thrive. (28)
What are the symptoms of erosive esophagitis?
Erosive esophagitis causes many of the same symptoms as other types of esophagitis, such as heartburn and difficulty or pain when swallowing. However, when left untreated, erosive esophagitis can lead to blood in vomit or stool. In severe cases it can lead to esophageal strictures, chronic inflammation and ulcers. (29)
What causes ulcers in the esophagus?
When acid from the stomach enters the esophagus because of GERD, it can eat away at the lining of the esophagus and cause an ulcer. Ulcers can also develop when certain kinds of pills are not rinsed down with enough water and saliva, leaving residue from the pill on the lining of the esophagus. (30) Other causes include smoking, too much alcohol, or infection with Helicobacter pylori, HIV, Candida, the herpes simplex virus or cytomegalovirus. (31)
What are the symptoms of esophageal cancer?
Esophageal cancer symptoms can sometimes be confused with the symptoms of regular esophagitis. (32) Signs and symptoms include: (33)
- Difficulty swallowing or choking on food
- Chest pain or burning
- Weight loss
- Cough that doesn’t go away
- Hoarseness
- Hiccups
- Bone pain
- Bleeding from the esophagus (this can show up in your stool and also cause you to feel tired)
It is very important to get medical attention if you think you have a symptom of esophagitis or esophageal cancer.

Causes & Risk Factors
In general, risk factors that may cause esophagitis include: (34)
- Vomiting
- Drinking alcohol
- Smoking
- A weakened immune system caused by medications or another health problem
- Taking pills without drinking enough water (especially alendronate, tetracycline, doxycycline, ibandronate, risedronate, potassium tablets and vitamin C tablets)
- Chest surgery or radiation therapy (for lung cancer, for example)
- Acid reflux (gastroesophageal reflux, or GERD)
- Allergies to food or things in the environment, such as pollen
However, risk factors vary by the type of esophagitis. For example:
- People with autoimmune conditions such as HIV are more likely to be affected by infectious esophagitis. (35)
- Reflux esophagitis is more common among people with GERD and those who eat shortly before bed, consume a lot of acidic foods or drinks including alcohol and caffeine, eat large and fatty meals, smoke, have excess weight, and consume other foods that can worsen GERD symptoms (tomatoes, citrus, garlic, mint, chocolate, etc.). (36)
- Eosinophilic esophagitis risk factors include food allergies and a family history of the condition, as well as male gender, white race and having other allergic issues (asthma, allergic rhinitis, or eczema). (37)
- Taking nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids or antibiotics increases the risk for drug-induced esophagitis. According to the Food and Drug Administration (FDA), the risks of NSAIDs include stomach and gastrointestinal problems when taken frequently; cases of esophagitis caused by NSAID use, and also that of antibiotics, can occur. (38, 39)
Conventional Treatment
Traditional medical treatment of esophagitis includes both over-the-counter (OTC) and prescription medications. Most physicians will also recommend lifestyle changes and solutions to help you minimize your symptoms naturally (see below). In serious cases, treatment of esophagitis strictures and esophageal narrowing may require surgery.
How do you treat esophagitis?
Generally, the type of medical treatment you receive will depend on the specific diagnosis you have. (40)
- Reflux esophagitis is typically treated with OTC or prescription antacids, proton pump inhibitors (PPIs), H-2-receptor blockers, or prokinetics. Surgery may help reduce acid reflux in severe cases.
- Eosinophilic esophagitis treatment typically involves avoiding the allergen, although you may also be prescribed proton pump inhibitors or steroids to coat your esophagus. If you need to identify food allergens, you may have to try an elimination or elemental diet as well.
- Drug-induced esophagitis treatment mostly involves taking replacement/alternative medications to reduce irritation. You can also improve your pill-taking strategies as a natural treatment (see below).
- Infectious esophagitis treatment requires treating the bacterium, virus, fungus or parasite that is causing the infection. The medication will target the underlying infection and once it is healed, the symptoms should go away.
How long does it take to recover from esophagitis?
How long esophagitis lasts depends on many factors, including the type and its underlying cause. People whose condition is caused by swallowing certain types of pills often experience relief within days of stopping the medication. People with infectious causes also experience swift relief with treatment.
However, reflux and eosinophilic esophagitis may last a long time — months or even years. Because they are caused by other problems that usually do not have a cure, such as food allergies, the esophagitis can often be managed but not cured. In these cases, treating esophagitis is essential to help minimize symptoms and avoid complications from the disease.
20+ Natural Ways to Manage Esophagitis Self-Care
The type of esophagitis treatment you pursue should be tailored to the diagnosis you have. For example, avoiding NSAIDs won’t make eosinophilic esophagitis go away. Work with your health care provider to come up with a plan for natural treatments for your specific type of esophagitis to help boost digestive health and immunity, in some cases.
General Self-Care (41)
- Take small bites of food, chew thoroughly (especially meats and firm vegetables) and drink plenty of water with pills or meals.
- Ask your physician if you can crush any pills that you take, or if liquid versions are available.
- Go to the emergency room for help dislodging any food that you cannot swallow or remove within one hour, or any stuck food that makes it hard to breathe. They can use a small tube to help remove the food or push it down into your stomach.
- Don’t smoke.
- Avoid medications that can cause or worsen esophagitis. Let your pharmacist and health care professional know about your diagnosis any time you get a new prescription or need to take an over-the-counter pill.
- Follow the steps for reflux self-care no matter what type of diagnosis you have, so that any acid reflux you may have will not make your condition worse.
Natural Reflux Esophagitis Self-Care (42)
- Avoid food and drinks that can aggravate acid reflux. Consider following a diet to reduce acid reflux or another esophagitis diet plan you develop with your health care provider.
- Eat several small meals throughout the day instead of two or three large meals.
- Stay upright for three hours after eating.
- Insert a wedge under the top of your bed (pillows don’t do the trick) to elevate your head at least 6 inches while you sleep.
- Limit alcohol intake.
- Lose excess weight.
- Consider herbal remedies to relieve or prevent heartburn and reflux, such as licorice, chamomile, slippery elm, marshmallow and more. Because these may interact with medications, always check with your doctor before using a new herb or supplement.
- Reduce stress and anxiety by exercising or using relaxation techniques to help reduce your reflux.
- Ask your health care provider whether acupuncture is safe for you. Provided you have no health reasons to avoid it, acupuncture may help reduce regurgitation and heartburn.
Natural Eosinophilic Esophagitis Self-Care
- Avoid the allergens causing your inflammation. If you do not know which foods or environmental allergens have caused your condition, ask your doctor about allergy testing. You can also work with a dietitian or allergist to do a formal elimination diet. (43)
- Follow the steps for naturally managing reflux esophagitis as well, since many people with eosinophilic esophagitis also experience some GERD symptoms that can make their condition worse. (44)
- Ask if you could benefit from an elemental diet, which replaces food with an amino acid-based formula. (45)
Natural Drug-Induced Esophagitis Self-Care (46, 47)
- Drink an entire glass of water each time you take a pill (including supplements and vitamins), unless your doctor tells you not to.
- Stay upright (sit or stand) for 30 minutes or more after taking a pill. This helps the pill reach your stomach and helps your saliva clear any residue from your esophagus.
- Ask your health care provider if you can stop or temporarily discontinue any medications you are on that may be causing the problem. You can also ask if a different medication can be taken or if a liquid version is available.
Natural Infectious Esophagitis Self-Care
- Take supplements and/or adjust your diet to help boost your immunity. However, always consult a health care professional before starting or stopping a supplement, since many natural compounds can interact with medications. (48)
- Consider taking a general multivitamin to make sure you do not have micronutrient deficiencies. (49)
- Ask your doctor if the top supplements that are believed to boost immunity may be beneficial for you. Popular choices include echinacea, ginger, probiotics, vitamin D and more.
- According to the Cleveland Clinic, you can also obtain immune system benefits from getting plenty of vitamins C, B6, and E in your diet. (50) Do this by eating plenty of green leafy vegetables, citrus fruits, salmon, tuna, chicken, chick peas, nuts and seeds.
- Ask your health care provider if you might benefit from dietary changes, such as an anti-inflammatory diet or a diet to help reduce yeast. (51)
- Dietary changes that may reduce inflammation include avoiding fried foods, refined carbohydrates, red meat, sugar-sweetened drinks, and animal fats. (52)
- Berries, nuts, seeds, fatty fish, olive oil, tomatoes and green leafy vegetables are believed to reduce inflammation. (53)
- Dietary changes to fight yeast overgrowth, in case your infection is related to yeast, include changes called the candida diet. Changes include following a low-sugar diet, using coconut oil as a mouthwash, and eating probiotics. (54)
- Stay hydrated and get plenty of rest to help you fight your infection. (55, 56)
- Ask your doctor if any immunosuppressant drugs you are taking can be reduced or eliminated. (57)
- Follow the natural treatment recommendations for reflux esophagitis as well. (58)
Precautions
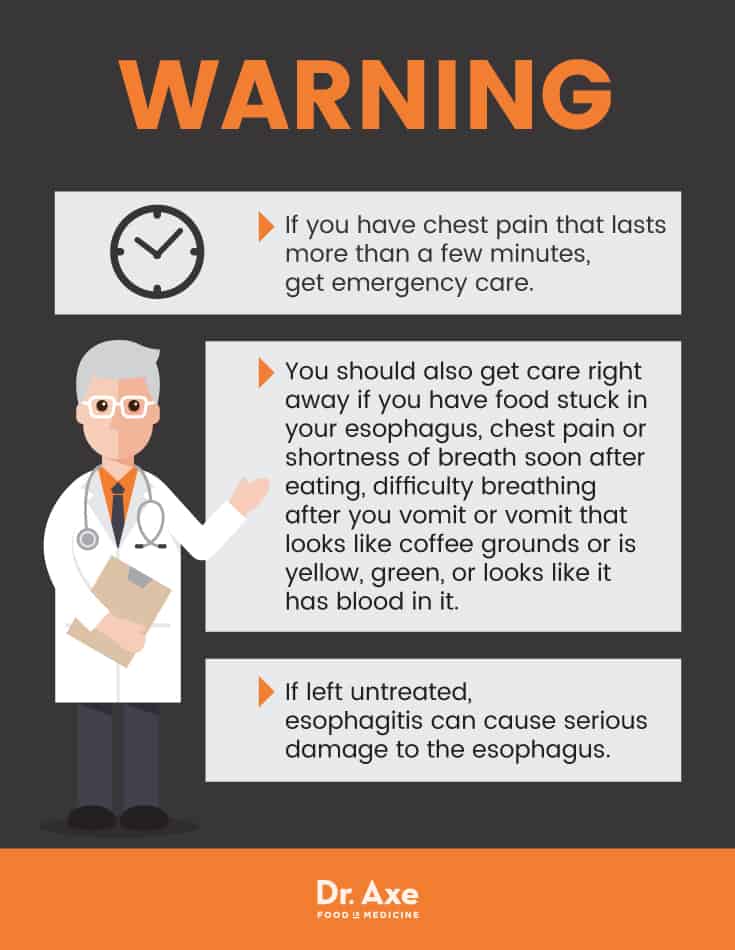
If you have chest pain that lasts more than a few minutes, get emergency care. You should also get care right away if you have food stuck in your esophagus; chest pain or shortness of breath soon after eating; difficulty breathing after you vomit or vomit that looks like coffee grounds or is yellow, green, or looks like it has blood in it.
If left untreated, esophagitis can cause serious damage to the esophagus. It can scar the tissue in the food pipe and make it narrower. These strictures can make it very difficult to swallow food. The lining of the esophagus can also be torn when food gets stuck and causes retching, or during an endoscopy if swelling is severe. Finally, untreated esophagitis increases your risk of Barrett’s esophagus. This is a condition in which cells of the esophagus start to change and increase your risk of esophageal cancer. (59)
Key Points
- When the lining of the food pipe gets irritated, swollen or inflamed, it is called esophagitis. In many cases, it has a cause that is fairly straightforward, such as infection or a food allergy.
- There are many natural ways to treat your symptoms and speed your healing.
- With proper management, this disease can either be resolved or at least held in check. However, some types are chronic and require long-term care and prevention efforts to avoid serious health problems.
- Do not attempt to self-diagnose your type of esophagitis.
- If you have esophagitis, follow the advice of your health care provider to treat it and to prevent complications now or in the future.
Each type of esophagitis may require unique natural therapies to improve symptoms. However, in general, there are some tips that may benefit your health if you have this diagnosis:
Natural Ways to Help Manage Esophagitis
- Take small bites of food and chew thoroughly to avoid choking.
- Drink plenty of water with pills or meals.
- Ask your physician if you can crush any pills that you take, or if liquid versions are available.
- Go to the emergency room for help dislodging any food that you cannot swallow within one hour, or that makes it hard to breathe.
- Don’t smoke.
- Avoid medications that can cause or worsen esophagitis.
- Follow the steps for reflux self-care, such as the GERD diet, raising the head of your bed, reducing stress, staying upright for three hours after eating.