This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
SI Joint Pain and Sacroiliitis: Causes, Natural Treatments and Exercises
February 19, 2019

Sacroiliac joint dysfunction, also commonly called SI joint pain, is a condition that causes upper leg and lower back pain. Studies show that low back and/or upper leg pains due to conditions like disc diseases, overuse, age-related degeneration of joints and inflammation are very common, affecting millions of people every year. In fact, in people over 45, low back pain is now the leading cause of disability and the second leading cause of doctor’s visits in the U.S.
Of all people with radiating back pain (the kind that runs down spinal nerves from the low back to the legs), between 15 percent to 30 percent experience symptoms due to sacroiliac dysfunctions. (1) Something unique about SI joint pain is that it commonly affects young and middle-aged women more than any other group. Onset of back and leg pain usually starts during someone’s 30s or 40s and can come and go for a the remainder of a person’s lifetime if he or she doesn’t take steps to resolve its underlying causes.
It’s often difficult for doctors to diagnose the exact cause of a patient’s back pain — for example, many people with sacroiliac joint problems are misdiagnosed with a herniated disc — because oftentimes the causes are multifactorial. However, in a high percentage of patients, disc degeneration and changes in the lower lumbar region of the back are contributing causes of low back/upper thigh pain, since this causes other joint compensations and postural problems.
If you’re suffering from low back/leg pain, here’s the good news: With treatment, up to 80 percent of all people with low back pain experience significant improvements in symptoms within about four to six weeks after diagnoses. What types of things can you do to help improve healing and treat discomfort caused by SI joint dysfunction? Natural remedies like stretching, resting, applying heat, prolotherapy and improving your posture can all offer relief.
What Is the Sacroiliac Joint?
The sacroiliac joint, also known as the SI joint, connects the pelvis with the lower spine. It carries the weight of the upper body and bridges it to the lower body. In fact, every person has two sacroiliac joints, which are located at the bottom of the spine right near the pelvis, sacrum, tailbone and hips. The lower part of the spine located down the back is known as the lumbar region, and the SI joints sit just below this area. (1)
The SI joints connect the pelvis bone (iliac bone) and sacrum (lowest part of the spine), absorbing shock and providing cushion between the bones, which allows for the hips to move. The sacrum or lower section of your spine is made of five non-moveable vertebrae alongside the two large hip bones called the ilium or iliac crests. (1)
The SI joint is an essential shock absorber during weight-bearing activities and also relieves some strain on the lower lumbar. According to a sports medicine study by Jack Harvey and Suzanne Tanner,
Lumbar spine pain accounts for 5 to 8% of athletic injuries. Although back pain is not the most common injury, it is one of the most challenging for sports physicians to clearly diagnose. Athletes who participate in sports involving repeated and forceful hyper-extension of the spine may suffer from lumbar facet syndrome, spondylolysis, or spondylolisthesis. (2)
The sacroiliac joint is surrounded by strong ligaments and muscles such as the erector spinae, psoas, quadratus lumborum, piriformis, abdominal obliques, gluteal muscles and hamstrings, all of which strengthen the SI joint. These surround and encapsulate the sacroiliac joint and all can be affected in sacroiliitis.
Normally the SI joints only move a small amount, so overuse can be one reason why pain occurs. When these joints become inflamed or degenerated over time for various reasons, triggering sensitivity and pain, a patient is then diagnosed with the condition called sacroiliitis.
What is sacroiliitis?
Medically speaking, the suffix “itis” refers to inflammation, while sacroiliitis refers to inflammation of the sacroiliac joint. Sacroiliitis is pain that could be dull or sharp and starts in your hip joint but can move to your buttocks, thighs, groin or upper back.
The pain may worsen when sitting for prolonged times and stiffness can be felt in the hips and lower spine. Sacroiliitis is a term that is sometimes used interchangeably with the term sacroiliac joint dysfunction. This can also lead to lower back pain and/or leg pain and can be caused by lumbar disc herniation or sciatica pain.
Why does SI joint pain and sacroiliitis happen?
Pain usually starts when your sacroiliac joint is inflamed or irritated. This inflammation is then classified as either acute or chronic. Acute inflammation is typically intense, short-lived and can be caused by an injury that heals in times as the pain gradually subsides. This can last anywhere from 10 days to six months. Chronic inflammatory pain is ongoing and may be mild or intense.
Sources of sacroiliac joint dysfunction usually include hypermobility/instability or opposite hypomobility/fixation. This pain can spread throughout your lower back, hips and legs. This pain becomes chronic after a patient experiences a prolonged level of pain that surpasses the acute phase.
There are several diagnostic tools that can be used such as x-rays, CT scans or MRI’s that can show the narrowing of the joint space or erosion of the bone area.
SI Joint Pain Symptoms, Causes and Risk Factors
Although some people experience pain in both legs or hips, most with SI dysfunction have symptoms in only one leg along with the low back.
The most common signs and symptoms of SI joint pain include:
- Low back pain
- Pain in the hips, butt or upper thighs — sometimes pain radiates down the legs, especially when moving, but usually stays above the knees
- Throbbing when exercising, bending, squatting, standing up from a sitting position, running or walking
- Reduced range of motion and limited flexibility
- Discomfort when sleeping on the painful side/hip or pain in certain lying positions
- Loss of balance/stability (some people feel like a leg is “giving out”)
- At times numbing, tingling or muscle weakness in the lower extremities
SI joint pain is primarily caused by: (3)
- Impact sports, weightlifting or falling down
- Repeated impact from activities like jogging or repetitive impact sports
- Pregnancy (when the body releases hormones that cause your joints to loosen up and move more, causing hypermobility)
- Illnesses like infection, arthritis and gout could cause inflammation
- Hyperactivity (moving the joints too much, especially in repetitive ways)
- Joint degeneration, sometimes caused by degenerative joint diseases, such as osteoarthritis
- Inflammation of the joint
- Hypomobility (loss of normal range of motion and movement)
- Poor posture, improper form and the SI joints overcompensating for other joints/body parts, which increases the amount of stress placed on them. For example, people with injuries to the lumbar region of the spine can lose normal range of motion in their backs, so the body then starts to compensate by placing more weight and pressure on the sacroiliac joints. This can also happen in those who haven’t healed well after lumbar surgery.
What sort of medical conditions or lifestyle factors make you more susceptible to developing SI joint pain?
Risk factors for sacroiliac joint dysfunction include:
- Being a woman: Women have broader pelvises, greater curvature of the lumbar spine and usually shorter limb lengths. Women also experience widening of the pelvis during pregnancy and increased pressure on the lower body (4)
- A history of other spinal diseases, arthritis, osteoarthritis or osteoporosis
- Major trauma or impact that causes injury to the ligaments and joints near the spine
- Smoking or using recreational drugs
- Long-term use of medications, including corticosteroids, or use of immunosuppresion drugs and chemotherapy
- Suffering from bacterial infections that affect the spine
- A history of cancer
- Pregnancy, which adds weight and pressure to the low back
- Being over the age of 50 makes you more likely to deal with spinal problems, such as a pinched nerve, due to the degenerative effects of aging. However, surveys show that young to middle-aged women frequently suffer from SI joint problems due to factors like postural problems, overuse and even pregnancy.
Diagnoses and Conventional Treatments
If you suspect the cause of your symptoms is a problem affecting the SI joint, visit your doctor for a physical examination. After ruling out “red flag” symptoms that suggest another type of disease could be to blame for your pain (such as bowel dysfunction or infection), you’ll likely receive a physical exam to test your range of motion, strength, flexibility, posture and symptoms when standing or sitting in different positions.
Because SI dysfunction can be hard to distinguish from other problems, your doctor might also choose to inject the SI joint with an anesthetic blocking drug in order to test your response and symptom improvements. (5)
NSAID pain relievers, and sometimes anesthetic injections or corticosteroids, remain the first-line treatment for most forms of spinal problems and disc diseases. NSAIDs help control inflammation and dull throbbing, but they usually don’t address the root cause of the problem and can cause side effects when used long term. For patients with severe pain, NSAIDs might need to be taken for long durations of time, or else symptoms will return. Problems associated with long-term NSAID use can include digestive discomfort, such as acid reflux, stomach ulcers, blood pressure changes, kidney problems and fluid retention. (6)
To recap, here’s the most common steps in conventional treatment of sacroiliitis:
- Physical therapy: PT improves strength and makes the joint more flexible to decrease the inflammation in the SI joint. This could also help correct any overcompensation habits created due to the pain. In conjunction, a therapist may use ultrasound, heat/cold treatments, massage and stretching.
- Injection: Shots of cortisone can be used to cut the inflammation to the joint. Some physicians will use a numbing solution such as lidocane or bupivacaine to relieve some of the pain.
- Rest: Utilizing a short period of rest along with heat and/or ice.
- Nerve treatment: Using a needle to permanently damage the nerves that send the pain signal to the SI joint and then to your brain.
- Surgical fusion of the SI joint: This is a very invasive procedure in which the sacroiliac joint gets surgically fused together. Both the nerve treatment and surgical intervention are considered last resort treatments.
Natural Treatments for SI Joint Pain and Sacroiliitis
1. Collagen Repair Diet
What is collagen, and how can it help you overcome joint pains? Collagen is the most abundant natural protein found within our bodies and an important building block of all tissue, including joints and ligaments. It can be found inside of joints and is one of the first things lost due to aging, overuse and inflammation.
The best natural source of collagen is real bone broth. Bone broth is high not only in collagen, but other beneficial substances like glucosamine, chondroitin, hyaluronic acid and amino acids, which help heal joint injuries.
Another way to help heal joints is to eat omega-3 foods (EPA/DHA). The best sources are wild-caught fish like salmon, mackerel and sardines, as well as other omega-3 foods like grass-fed beef, chia and flaxseeds. All of these are beneficial for fighting inflammation and many different age-related problems.
Consume more antioxidants and anti-inflammatory foods, which support tissue repair. These include organic vegetables, organic fruits, and herbs like turmeric, ginger, garlic, etc.
2. Posture Correction Exercises and Physical Therapy
Proper posture when standing or sitting/working along with using the right form when exercising are both crucial for keeping unwanted stress off of joints. It’s possible that your sacroiliac pain is caused due to muscular/joint compensations, especially those stemming from abnormalities in the lower lumbar region.
To help overcome this, I recommend seeing a physical therapist, an Egoscue posture therapist and/or a spinal correction chiropractic doctor from the Clear Institute (especially if you suffer from conditions like scoliosis). These professionals can help correct poor postural problems, such as forward head posture, and reteach you how to position your weight correctly.
These treatments are especially helpful if your SI joint is “stuck” in an abnormal position or hypermobile and unable to move normally. The types of chiropractic adjustments you can expect to receive for SI joint pain include side-posture manipulation, drop technique, blocking techniques and instrument guided methods. (7)
3. Prolotherapy (PRP) Treatments
Prolotherapy is a cutting-edge form of regenerative medicine that’s leading the way in helping both acute and chronic injuries. Studies have found that prolotherapy is one of the most useful and effective forms of treatment in SI joint pain patients because not only does it improve tissue healing, but it can help boost effectiveness of exercises/stretches that balance the trunk and lower extremities. (8)
Many elite athletes are now even turning to PRP treatments (those using platelet-rich plasma) to manage painful symptoms due to arthritis, a torn ligament, tendonitis, bulging disc, or pain in any joint, such as the neck, low back, knee or shoulders. What is prolotherapy exactly, and and how does PRP work?
Prolotherapy uses your body’s own natural platelets and growth factors to heal damaged tissues. A form of stem cell therapy, this is quickly becoming viewed as one of the most advanced forms of regenerative medicine for treating inflammatory conditions or overuse/trauma injuries. I recommend the brand Regenexx, which I personally use, as has my wife for past injuries.
4. Soft Tissue Therapy
By helping you overcome compensations, poor posture/form when exercising and overuse, soft tissue practitioners can aid in eliminating muscular pain. I’ve used active release technique (ART) practitioners for years to help me overcome a number of muscle- and joint-related injuries. What does soft tissue therapy do to resolve pain? It can relieve tight muscles, scar tissue that has formed in myofascial tissue and painful trigger points in order to reduce joint stress.
Consider visiting a specialist in ART, Graston Technique®, dry needling and neurokinetic therapy.
5. Supplements to Reduce Inflammation
Because many people are low in nutrients that help preserve joint health and prevent deterioration of the musculoskeletal system, taking certain supplements can be very helpful. In order to heal damaged tissues, you need nutrients that help reduce inflammation, support tissue repair and increase growth factors.
The following supplements are useful for overcoming SI joint pain:
- Turmeric essential oil: this ancient herb has healing properties and contains an active ingredient called curcumin. One study published in the Journal of Agricultural and Food Chemistry evaluated the anti-arthritic effects of turmeric essential oil and found that crude turmeric essential oil given orally at a dose that would correspond to 5,000 milligrams per day in humans had a modest anti-inflammatory effect on the joints of animal subjects. (3)
- Ginger
- Bromelain
- Omega-3 supplements
- Protein powder made from bone broth: contains type 2 collagen, glucosamine, chondroitin and hyaluronic acid. These can aid in tissue repair, as can bovine collagen powder, which has type 1 and 3 collagen.
- Antioxidant-boosting compounds: These include resveratrol, green tea, cordyceps and berry extracts. Antioxidants can help support the body’s own stem-cell production and initiate tissue regeneration.
6. Rest and Apply Heat/Ice to Reduce Pain
To help dull pain, apply heat (or ice if you’ve experienced an injury) to the affected area for 15—20 minutes at a time, up to several times daily. Icing the area is best during the first two days to two weeks following trauma or an injury, but during this time avoid heating, which can make inflammation worse.
SI Joint Pain Exercises and Stretches
Once your condition has healed enough for you exercise, get clearance from your doctor and work on strengthening the muscles near the SI joint. This can include doing low-impact bodyweight exercises, gentler exercise like tai chi, brisk walking or water aerobics.
Low-impact exercise is part of ongoing maintenance for healthy joints, since it helps bring blood to the damaged area, controls inflammation, and improves balance and flexibility. Exercises that bring the knees toward the chest and rotate the lumbar region are especially important for stretching the SI joint.
To better support and strengthen the sacroiliac joint and pelvis/lower back area, an athlete can focus on gaining core strength both anteriorly and posteriorly.
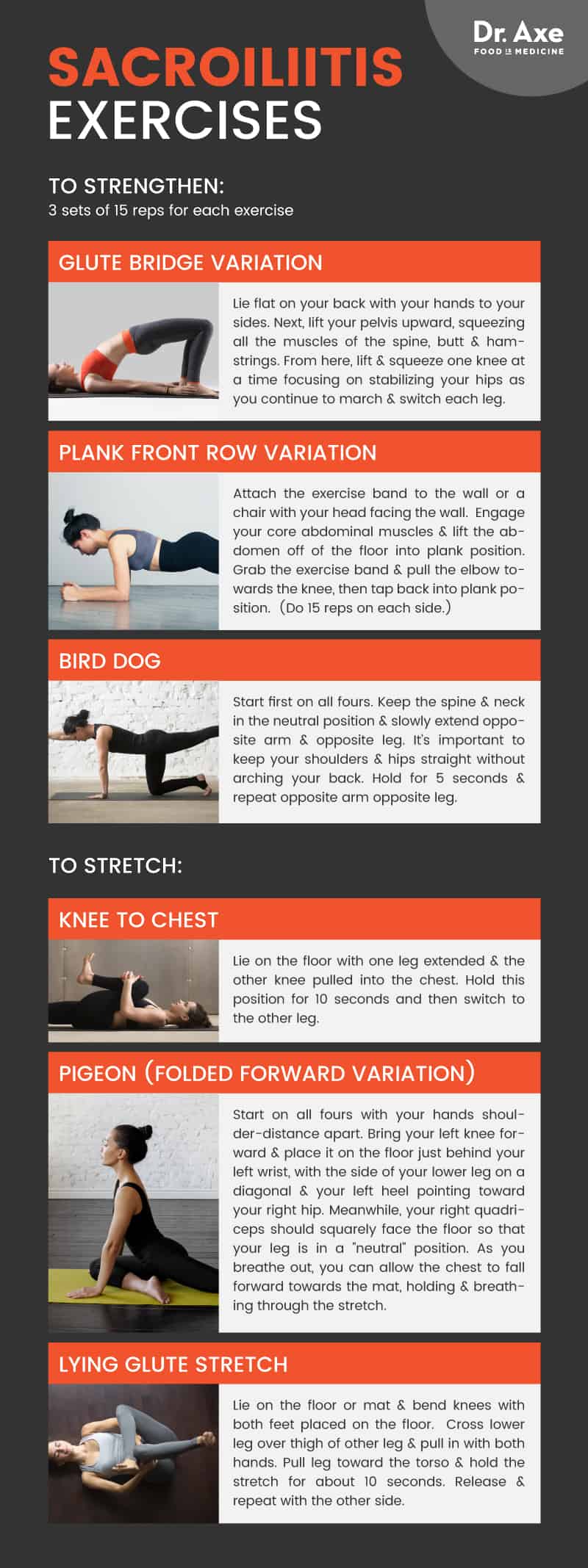
Here are some SI joint strengthening exercises:
- Glute Bridge Variation: Lie flat on your back with your hands to your sides. Next, lift your pelvis upward, squeezing all the muscles of the spine, the glutes and posterior legs. From here, lift and squeeze one knee at a time, focusing on stabilizing your hips as you continue to march and switch each leg. Repeat this exercise for 3 sets of 15 reps.
- Plank Front Row Variation (with exercise bands): Attach the exercise band to the wall or a chair with your head facing the wall. Engage your core abdominal muscles and lift the abdomen off of the floor into plank position. Grab the exercise band and pull the elbow towards the knee, then tap back into plank position. (Do 15 reps on each side.)
- Bird Dog: This will work your lower back and core abdominal muscles in addition to helping stabilize the muscles of the spine. Start first on all fours. Keep the spine and neck in the neutral position and slowly extend opposite arm and opposite leg. It’s important to keep your shoulders and hips straight without arching your back. Hold for 5 seconds and repeat opposite arm opposite leg.
SI joint stretches will help reduce muscle tension and spasms in the lower lumbar, which could be leading to the acute or chronic hip/lower back pain:
- Knee to Chest: Lie on the floor with one leg extended and the other knee pulled into the chest. Hold this position for 10 seconds and then switch to the other leg.
- Pigeon (Folded Forward Variation): Start on all fours with your hands shoulder-distance apart. Bring your left knee forward and place it on the floor just behind your left wrist, with the side of your lower leg on a diagonal and your left heel pointing toward your right hip. Meanwhile, your right quadriceps should squarely face the floor so that your leg is in a “neutral” position. As you breathe out, you can allow the chest to fall forward towards the mat, holding and breathing through the stretch.
- Lying Glute Stretch: Lie on the floor or mat and bend knees with both feet placed on the floor. Cross lower leg over thigh of other leg and pull in with both hands. Pull leg toward the torso and hold the stretch for about 10 seconds. Release and repeat with the other side.
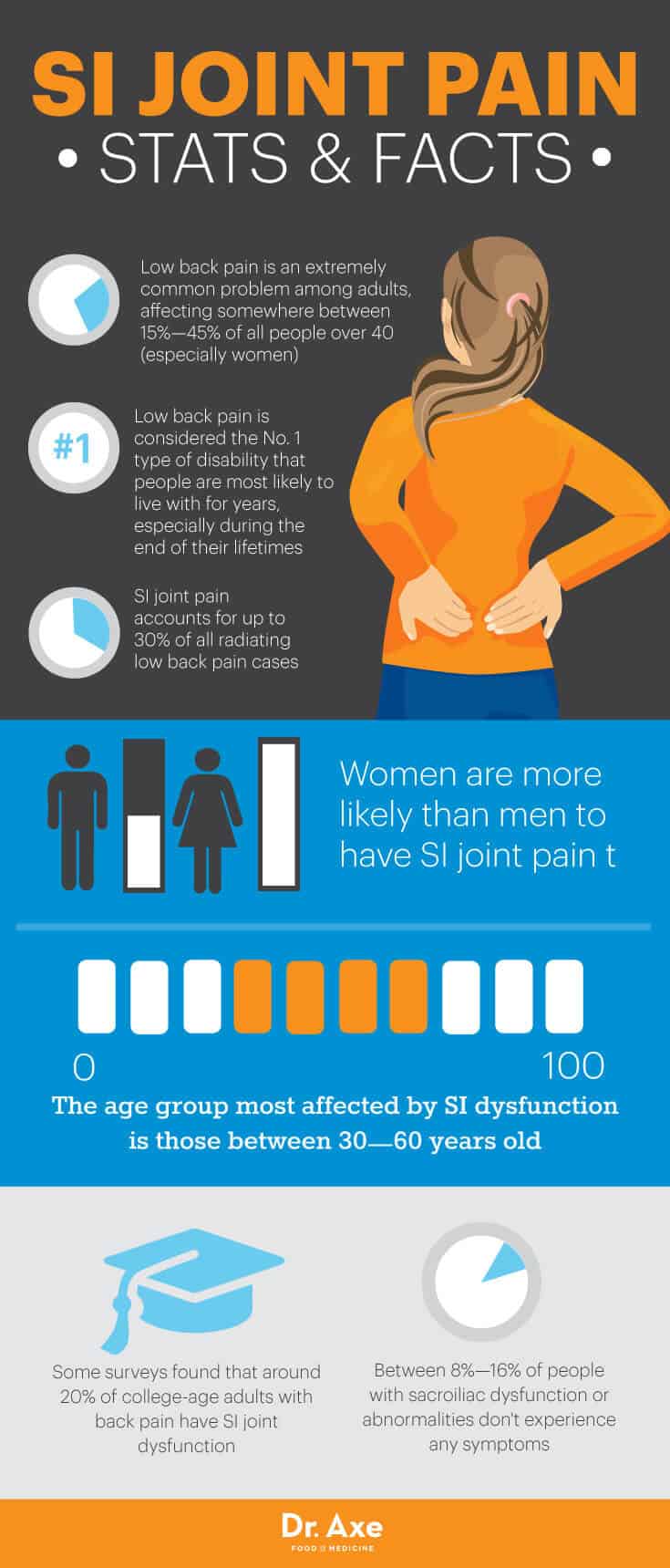
Sacroiliac Joint Pain Statistics
- Low back pain is an extremely common problem among adults, affecting somewhere between 15 percent to 45 percent of all people over 40 (especially women).
- Low back pain is considered the No. 1 type of disability that people are most likely to live with for years, especially during the end of their lifetimes.
- SI joint pain accounts for up to 30 percent of all radiating low back pain cases. (9)
- Women are more likely than men to have SI joint pain. The age group most affected by SI dysfunction is those 30–60 years old.
- Some surveys found that around 20 percent of college-age adults with back pain have SI joint dysfunction. (10)
- Between 8 percent and 16 percent of people with sacroiliac dysfunction or abnormalities don’t experience any symptoms.
SI Joint Pain vs. Other Spinal Disk or Joint Diseases
What makes sacroiliac pain different from other common causes of back pain, like arthritis or sciatica, for example?
- Sacroiliac dysfunction remains difficult to diagnose in many cases and has a lot of overlap with disc herniation and radiculopathy (pain that runs down the back along the sciatic nerve). The good news is that although SI pain can falsely be attributed to a herniated disc in some patients, treatments for both conditions are similar.
- Common joint disorders, such as rheumatoid arthritis, usually affect the cervical part of some joints (mostly in the knees, hands or feet) and don’t commonly impact the SI joint.
- Other health problems that can contribute to spinal disc problems might also cause bowel/digestive dysfunction, morning stiffness and skin inflammation, which aren’t common in sacroiliitis.
- If your back/leg pain feels the worst when you wake up in the morning but gets better when you move more, it likely isn’t the sacroiliitis causing your problems, but possibly arthritis, an infection or another inflammatory disorder.
- If you feel pain running down the back of your legs that extends to your ankle or foot, you might have sciatic nerve pain. SI joint pain is similar to sciatica, but the two have different causes (sciatica pain radiates down the sciatic nerve located in the lower back).
Precautions
SI joint dysfunction is certainly not the only reason you might be feeling lower back or leg pain, so it’s always best to get a proper diagnosis from a doctor before taking any steps to treat your condition. If you developed back pain prior to being 30 years old and experience other symptoms — such as morning stiffness, unexplained weight loss, bowel problems, fever, rashes, pain that lasts for more than six weeks and pain that improves with activity — it’s possible that the real cause for your pain is another disorder or disk disease.
Final Thoughts
- The sacroiliac joint (SI joint) is located at the bottom of the spine right near the pelvis, sacrum, tailbone and hips.
- Dysfunction of the SI joint can cause pain and limited range of motion in the lower half of the body, especially the low back, hips, buttocks and upper thighs.
- Causes of SI pain include degenerative joint diseases, poor posture, added pressure due to pregnancy, overuses and other injuries affecting the spine.
- Natural treatment for SI joint pain include prolotherapy, a diet rich in collagen, soft tissue therapies, physical therapy, low-impact exercise and chiropractic adjustments.



