This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Get Your Life Back: 5 Natural Treatments for PTSD Symptoms
March 9, 2021
About 70 percent of adults in the U.S. will experience some type of traumatic event at some point in their lives, and among these people about 20 percent will go on to develop the condition called post-traumatic stress disorder (PTSD) and experience PTSD symptoms.
The U.S Department of Veteran Affairs states that PTSD is a mental health problem that commonly occurs in veterans following combat. However, someone certainly doesn’t have to serve in the military to deal with symptoms of post-traumatic stress.
PTSD symptoms can affect both children and adults who have dealt with completely different types of traumatizing events. Risk factors for suffering from PTSD include:
- surviving a natural disaster
- getting into a car accident
- dealing with a sudden illness or injury
- suffering from abuse, neglect, domestic violence, violence, poverty or sexual assault
Mental health professionals who treat patients with PTSD typically use a combination of approaches to help their patients manage PTSD symptoms like anxiety, insomnia, depression and social isolation. These can include medications (when needed), “talk therapy” or counseling, group support, and other natural outlets for negative emotions, like exercise or meditation.
Related: What Is Autophobia? How to Treat the Fear of Being Alone
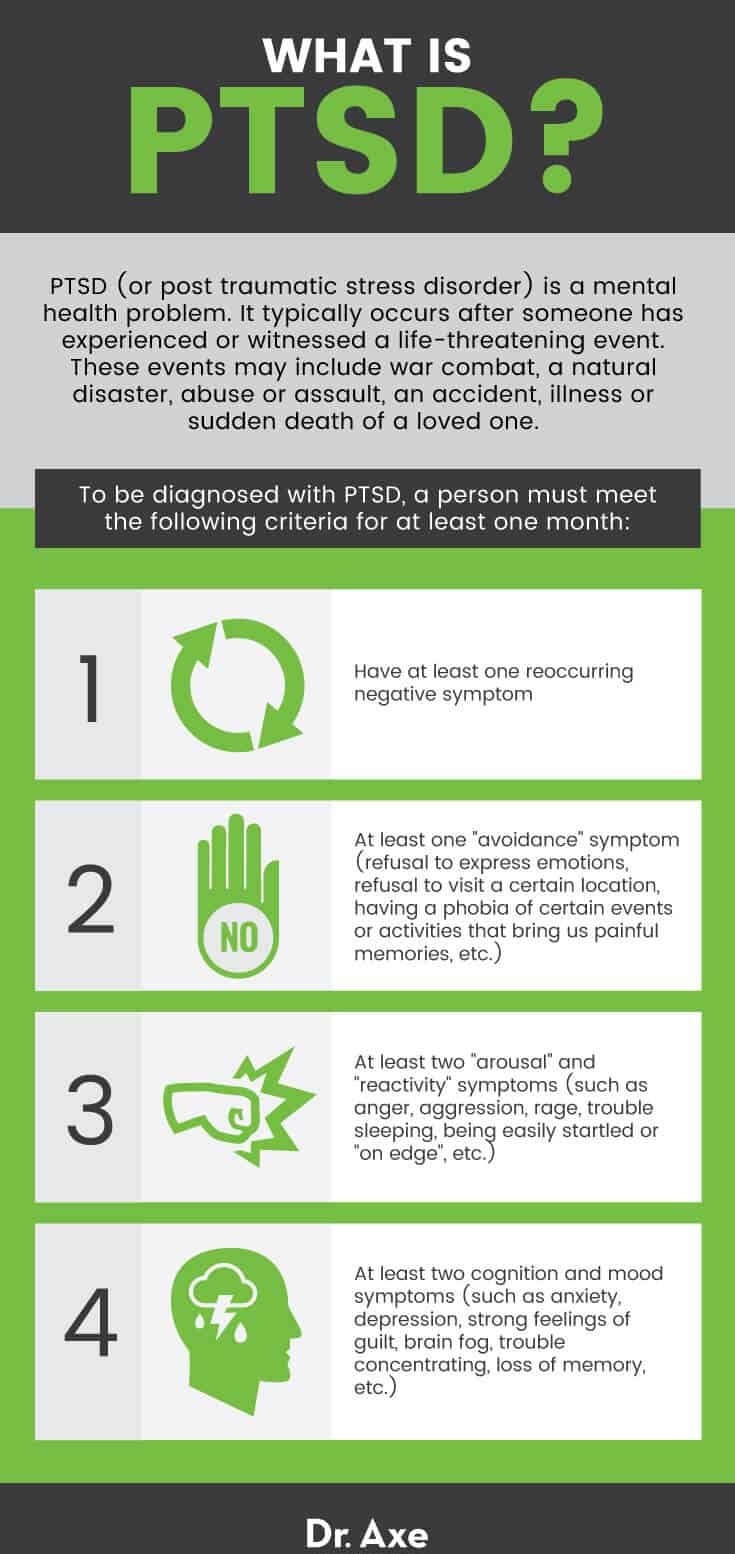
What Is PTSD?
Post-traumatic stress disorder is a mental health problem that is defined as “psychiatric disorder that may occur in people who have experienced or witnessed a traumatic event such as a natural disaster, a serious accident, a terrorist act, war/combat, or rape or who have been threatened with death, sexual violence or serious injury.”
According to a 2019 report in World Psychiatry, it’s the most common psychiatric disorder experienced by people exposed to trauma. It affects about 3 percent to 4 percent of the U.S population.
What does PTSD do to a person? Trauma can haunt a person after experiencing one or more difficult and painful events, affecting that person’s ability to live a normal, daily life by increasing PTSD symptoms like anxiety.
To officially be diagnosed with PTSD, a person must meet the following criteria for at least one month:
- Have at least one reoccurring negative symptom
- At least one “avoidance” symptom (refusal to express emotions, refusal to visit a certain location, having a phobia of certain events or activities that bring us painful memories, etc.)
- At least two “arousal” and “reactivity” symptoms (such as anger, aggression, rage, trouble sleeping, being easily startled or “on edge,” etc.)
- At least two cognition and mood symptoms (such as anxiety, depression, strong feelings of guilt, brain fog, trouble concentrating, loss of memory, etc.)
Related: Classical Conditioning: How It Works + Potential Benefits
Link to Nutrition
News published in 2020 by the University of Toronto found that there’s often a link between poor nutrition and experiences of PTSD. Among Canadians between the ages of 45 and 85, adults were less likely to exhibit PTSD if they consumed an average of two to three fiber sources daily.
Dietary fiber is believed by researchers to have some mental health-related protective effects due to the communication network that connects the gut and brain.
Eating a fiber-rich diet has beneficial effects on metabolic byproducts of bacterial fermentation made by microbes in the human gut. These byproducts affect how cells in the brain may work.
Daily consumption of pastries, sugary pulses, nuts, including peanut butter, and chocolate was associated with increased risk for PTSD.
Other risk factors that may be related to nutrition that increase the odds of someone developing PTSD symptoms include:
- being a racialized immigrant
- being a woman living in poverty (women had almost double the prevalence of PTSD in comparison to men)
- having chronic pain
- having a history of smoking
Related: How Dialectical Behavior Therapy (DBT) Works + Benefits
PTSD Symptoms
The majority of people who have “normal” coping mechanisms usually recover from initial symptoms of shock or sadness within a short time period. What makes PTSD symptoms different from negative emotions that are considered normal aspects of grief or healing?
In those who don’t have PTSD, an upsetting or dangerous event can cause serious symptoms, but the symptoms usually go away after a few weeks. (This is called acute stress disorder.) On the contrary, long after the dangerous or upsetting event is over, people with post-traumatic stress still feel very anxious, unable to express themselves and in general “not themselves.”
What are the four types of PTSD symptoms? They are generally grouped into four types:
- intrusive memories
- avoidance
- negative changes in thinking and mood
- changes in physical and emotional reactions
In order to be diagnosed with PTSD, a patient’s symptoms must:
- Meet the criteria described above
- Last more than one month
- Be severe enough to interfere with relationships or work
- According to experts, PTSD is often (but not always) accompanied by changes in mood. These changes may include depression, anxiety, social isolation and substance abuse.
What are the symptoms of PTSD?
According to the Anxiety and Depression Association of America, some of the most common PTSD symptoms include:
- Having flashbacks (reliving the trauma via memories and bodily sensations over and over again)
- Physical symptoms of anxiety, including a racing heart, sweating, inability to think clearly, etc.
- Nightmares or strange dreams, insomnia, and difficulty getting enough rest
- Having frightening thoughts that appear to come out of nowhere and last for several hours
- Feeling very anxious when encountering images, words, objects or situations that are reminders of the traumatic event
- Guilt and shame, which leads to avoiding talking to anybody else about thoughts or feelings
- Refusal to do certain things or making changes in one’s personal routine in order to avoid scary triggers or memories (this can include driving, going on vacation, being in an intimate relationship, etc.)
- Being tense, on edge and easily startled
- Having angry outbursts and sometimes being violent or aggressive with family and strangers
- Sometimes difficulty having a normal job, completing tasks due to lack of concentration, learning, and remembering new or old information (these are common “complex PTSD symptoms”)
- Other symptoms tied to high stress levels, such as changes in appetite or weight, headaches, digestive issues, and skin irritation
- Higher risk for substance abuse (including medications, drugs or alcohol)
- Depression (ongoing negative thoughts about oneself or the world), distorted feelings of guilt or blame, social isolation due to feeling alienated or misunderstood, loss of interest in enjoyable activities or hobbies due to low motivation, and in severe cases suicidal thoughts
- Children suffering from PTSD can also deal with symptoms like inability to open up to others or connect, trouble sleeping, difficulty learning, bed-wetting, or acting very “clingy” with caregivers.
- Teens can sometimes cause problems in school, be disrespectful to teachers or authority figures, be aggressive and violent, or develop eating disorders. In fact, PTSD is often a co-occurrence among those who suffer from eating disorders or other issues, commonly that have roots in sexual abuse or other types of childhood trauma.
What are the stages of PTSD?
PTSD symptoms usually begin shortly after the event takes place. Typically symptoms start within three months and last for up to a year.
However, sometimes abnormal symptoms might not appear for up to several years after the event has ended. This delay can sometimes make seeking help and getting a proper diagnosis a complicated issue.
Some experts consider PTSD to be divided into four phases:
- the impact phase (initial reactions of shock)
- the rescue phase (coming to terms with what happened)
- the intermediate recovery phase (adjusting to life following trauma)
- the long-term reconstruction phase (rebuilding and continuing to deal with the aftermath)
How long do PTSD symptoms last?
Every person has a different experience. Some overcome their symptoms and reach a stage considered to be “recovery” within about six months.
Others with “complex PTSD symptoms” deal with symptoms such as anxiety, guilt, shame, isolation and suicidal thoughts for years. Complex PTSD symptoms usually result from trauma that happened early in life (such as by a parent), happened for a long time and happened when the victim was alone.
Getting help from a mental health professional, seeking support from a group of peers or family and friends, and sometimes considering medication can all decrease the odds that PTSD will remain chronic and debilitating for many years.
Related: What Is Psychodynamic Therapy? Types, Techniques & Benefits
 Related: Somatic Experiencing Therapy: How It Works & How to Do It
Related: Somatic Experiencing Therapy: How It Works & How to Do It
Causes and Risk Factors
Risk factors for post-traumatic stress disorder:
This disorder typically occurs after someone has experienced or witnessed a life-threatening event. These events may include war combat, a natural disaster, abuse or assault, an accident, illness, or sudden death of a loved one.
As mentioned earlier, those who are more likely to struggle with PTSD include:
- War veterans
- Children and adults who have been through physical or sexual assault
- Those who have dealt with any type of abuse, accidents, natural disasters, terrorist attacks, political violence, death of a loved one, a serious illness or injury, or many other types of traumatizing events that seem “out of their control”
- A history of substance abuse or using drugs
- Women are more likely to develop PTSD than men, although it’s not exactly clear why. A high risk factor for women is having a history of sexual assault and rape.
- Genetics also seem to play a role in mental illnesses, including anxiety, depression and PTSD. A family history of mental illness can make some people more likely to develop PTSD than others, especially when combined with other risk factors.
- Being middle-aged
- Living in poverty
- Being an immigrant
- Experiencing racism
- Not being able to work
- Having chronic pain
Changes in the brain due to trauma:
Researchers, including neuroscientists (who study the brain) and psychotherapists (who study maladaptive behaviors), have found that people with PTSD display abnormal levels of certain stress hormones, in addition to experiencing changes in brain activity.
- Adrenaline, the hormone that helps kickstart the “fight or flight response” in response to danger, has been shown to remain elevated in people with PTSD long after the event has ended. This reaction is different than what occurs in people without PTSD.
- The perception of danger or fear triggers many split-second changes in the body and brain, evoking the fight-or-flight response. This can cause the person’s heart rate to speed up, breathing to get faster, the pupils in the eyes to dilate, perspiration to increase and digestion to slow down.
- These physiological symptoms tied to stress will continue for many months, even years, in people experiencing PTSD. Stress hormones will also spike very quickly and disproportionately in response to even mildly stressful stimuli.
- Constantly elevated stress hormones negatively impact the entire body, including memory, emotion regulation and attention. The result is high levels of irritability, muscle tension, trouble sleeping, heart problems and many other long-term health issues.
Other neurological and biochemical changes have also been shown to take place in the brains and bodies of those with PTSD, including in the limbic system (the primal, emotional center of the brain). Studies suggest that three of the primary areas impacted by trauma include:
- Amygdala
- Hippocampus
- Pre-frontal cortex
Changes in the brain following traumatic events can even be similar to the types of neurological changes seen in patients with brain injuries due to impact, accidents, etc.
Essentially, PTSD occurs due to loss of normal “executive functioning.” In other words, it occurs due to a loss of the ability to identify cause and effect, grasp the long-term effects of behaviors or actions, and create plans for the future.
Past trauma may make someone less intuitive, emotional, visual, spatial and tactual but more sequential and analytical.
Changes in brain activity, including deactivation of the left hemisphere, directly impact the capacity to organize past experiences, put them into logical sequences, and translate shifting feelings and perceptions into words that can be expressed to others.
Treatment
Conventional Treatment for Post-Traumatic Stress Disorder:
- The most studied type of treatment for PTSD is use of prescription medications, especially antidepressants. Most experts believe that medications work best when combined with psychotherapy in order to help patients feel more in control of their recovery.
- Drugs intended for PTSD are used to help patients deal with feelings of anxiety, sadness, anger, lack of motivation, feeling numb inside, social isolation, etc.
- Antidepressants for PTSD include several types of selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs). These are used to treat depression in general, including in patients who do not have PTSD but suffer from similar symptoms. One medication called Prazosin is commonly prescribed for PTSD symptoms tied to anxiety and depression, including physical reactions, nightmares and helplessness.
- While side effects are always possible when using medications, they can also be life-saving for some patients. They can also be an important catalyst toward recovery while beginning other natural treatments. Medications will not work for every patient. There are no guarantees, and there is a wide array of reactions depending on the specific drug.
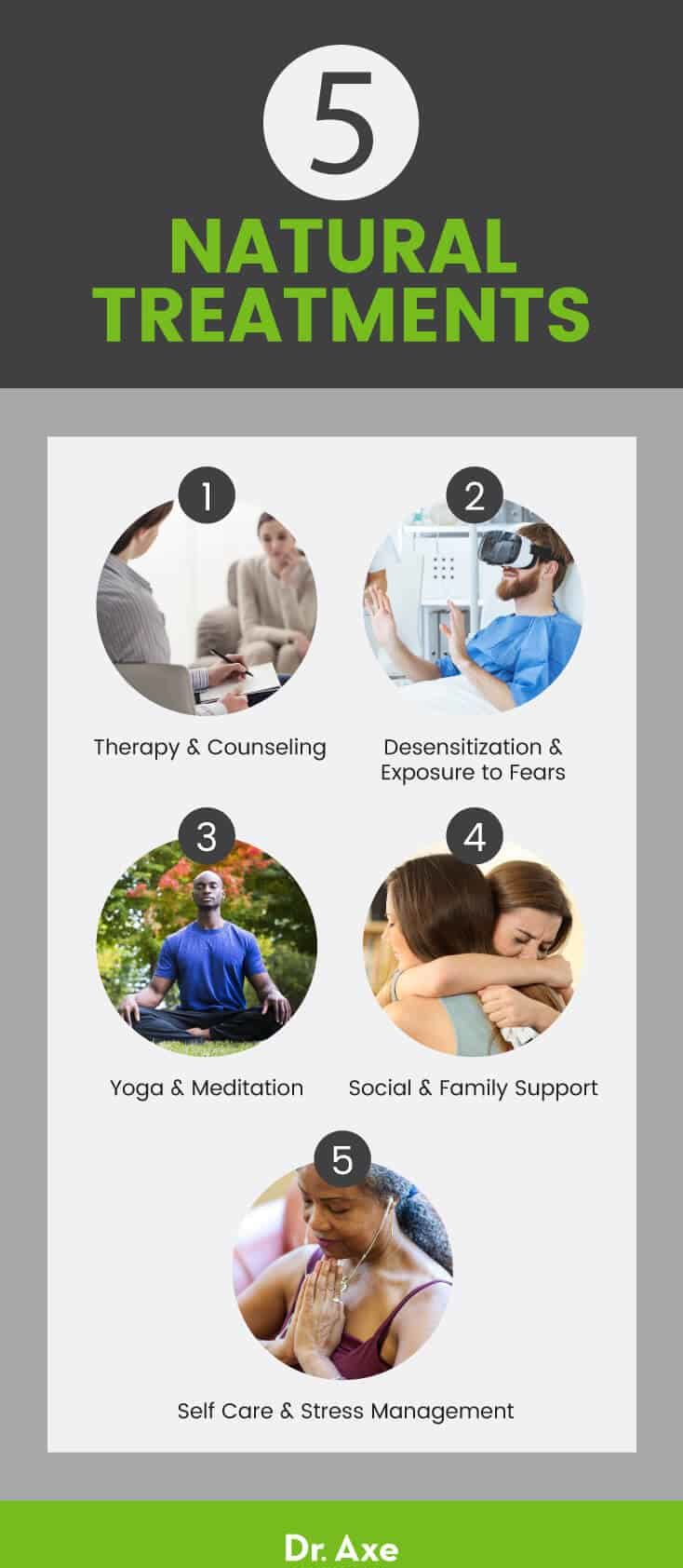
Natural Treatments for PTSD:
1. Therapy and Counseling
If you suspect that you or someone you know is suffering from PTSD, it’s best to reach out for help right away. When feelings become unbearable and interfere with normal life, ask a family member, teacher or your doctor for help.
You can refer to the National Institute of Mental Health’s Help for Mental Illnesses page to find a qualified mental health provider or social services worker in your area. In the case of an emergency (such as during a period of panic or major depression), an emergency room doctor can also provide temporary help.
Various types of psychotherapy (talk therapy) are used to help people overcome PTSD. The type of therapy depends on the situation and access to professional care.
Although many patients report experiencing increased distress during initial therapy sessions, as they get accustomed to discussing traumatic memories, one study found that talking about trauma in therapy sessions resulted in 86 percent of participants showing improvement in their PTSD and psychotic symptoms by the end of treatment.
One type that has been shown to be very effective is cognitive behavioral therapy (CBT) in which thoughts are examined in order to determine how they affect behaviors and self-perception.
Some of the primary goals of therapy for PTSD include:
- Training a patient to better access the “emotional brain” that has been cut off. Many with PTSD feel “numb” and cannot tie events to emotions. A therapist can help patients open up about how they’re really feeling and form connections.
- Increasing self-awareness. A therapist can teach patients skills to understand how trauma changed their thoughts and feelings, in addition to how it impacts their bodies and health.
- Regaining a feeling of having control over one’s own life.
- Helping develop coping strategies for dealing with difficult emotions.
Therapists often work with patients with PTSD to help them learn to become more aware of their inner experience and to begin to befriend what is going on inside themselves. This includes physical sensations, emotions and thoughts.
Learning from past experiences and better vocalizing of feelings are other important areas to address. This is because helplessness and social withdrawal are both very common with PTSD.
2. Desensitization and Exposure to Fears
In addition to common types of talk therapy, several forms of exposure therapy are also used to desensitize patients to perceived threats, relieve stress and help them to face fears directly. A professional therapist usually conducts exposure therapy. The therapist can be a guide as the patient gradually faces situations, objects or locations that bring up strong feelings of the traumatic event.
- Prolonged Exposure — This is a type of therapy that involves discussing, facing and recalling the traumatic event in detail in order to gain control over upsetting thoughts, physical reactions and feelings about the trauma. The idea is that the more someone discusses the upsetting event, the more familiar it becomes and therefore the less feared. There are different ways to expose the patient to their fears. These include using imagining, writing, drawing or painting, or visiting the place where the event happened.
- Cognitive restructuring — This approach is similar to CBT and other forms of exposure therapy. It helps people make sense of the bad memories by discussing them. Feelings of regret, guilt and shame are often a central component to talk about since they can contribute to the patient feeling “stuck.”
- Eye Movement Desensitization and Reprocessing (EMDR) — EMDR therapy involves having the patient focus attention on physical movement or sensations (like breath, sounds or hand movements) while he or she recalls the trauma and talks about it openly. By doing this, the patient has something to ground her/his attention in order to help the brain work through the traumatic memories.
3. Yoga and Meditation
In research supported by the National Institutes of Health, patients who took part in a 10-week program including yoga and mind-body practices on average experienced markedly reduced PTSD symptoms, even patients who had failed to respond to any previously used medications.
Yoga has been shown to change the brain by helping increase “happy” neurotransmitters, reducing the effects of stress, helping improve coping mechanisms for negative feelings and more. Participants in the study learned ways to help increase five specific types of positive, comforting feelings.
These feelings are GRACE:
- gratitude and compassion
- relatedness
- acceptance
- centeredness
- empowerment
Research suggests that another reason yoga and other forms of mind-body practices work so well for reducing PTSD symptoms is because they positively impact the nervous system. This is because they can change chemical signals sent via the vagus nerve back to the brain, helping promote relaxation.
Some of the ways that PTSD patients can directly tap in to their bodies’ “relaxation response” include:
- controlled breathing
- stretching or moving in purposeful ways (i.e., yoga asanas)
- chanting songs or mantras with a group
- practicing dozens of styles of meditation
There is also a lot of emerging data supporting mindfulness and meditation as an effective treatment approach for patients with PTSD due to how “neuroplasticity” (the brain’s ability to change itself based on repetition and focused attention) can improve neurological processes.
4. Social and Family Support
One of the strongest predictors of being able to overcome symptoms of PTSD is “building resilience” through social support and close relationships. Certain factors can help increase resilience, including:
- Joining a support group, which helps decrease feelings of isolation and alienation by opening up to others and forming compassionate relationships
- Visiting a family therapist in order to increase support from family, spouses, children or close friends
- Finding a spiritual or faith-based support group that can offer encouragement, an outlet, hope and positive feedback
- Social support also helps reduce aggression. It teaches those with PTSD how to respond to fear or other negative feelings without shutting others out. It also can give life a sense of purpose or meaning.
5. Self-Care and Stress Management
In addition to getting support from others, self-care is crucial for managing stress and triggers. Experts recommend some of these strategies:
- Eating a healthy diet that is low in sugar and processed foods but high in fiber (such as from vegetables, fruits, whole grains, beans, legumes, nuts and seeds)
- Engaging in regular, but usually mild, physical activity or exercise
- Getting enough sleep and downtime
- Being patient, including having realistic goals for how long it can take to feel better
- Reducing work-related stress and not taking on too much at once
- Spending more time in nature and with other people who help you feel comforted
- Becoming more knowledgeable about the condition through reading, journaling, speaking with a professional, videos, podcasts, etc.
Related: Systematic Desensitization Benefits + How to Do It
Conclusion
- PTSD is a mental health disorder that affects 7 percent to 8 percent of the population, including children and teens.
- It typically occurs after someone has experienced or witnessed a life-threatening event. These events may include war combat, a natural disaster, abuse or assault, an accident, illness, or sudden death of a loved one.
- PTSD symptoms include anxiety, depression, social isolation, sleep trouble and nightmares, guilt and shame, aggression, and avoiding talking to anybody else about thoughts or feelings.
- Treatments for PTSD include use of medications, therapy or counseling; group and family support; yoga; exercise; meditation; and other forms of managing stress through self-care.








