This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Pulmonary Embolism Prevention + 5 Natural Remedies
February 25, 2017
About half of all people who have pulmonary embolism (PE) display virtually no symptoms, the National Heart, Lung, and Blood Institute reports. In fact, many aren’t aware at all of having the condition. (1) The number of people affected by PE and deep vein thrombosis is between 300,000-600,000 people each year in the United States alone. (2)
Pulmonary embolism is life-threatening and very serious regardless of which symptoms are present. One of the scariest things about pulmonary embolism is that it can cause immediate reactions without any warning signs. When someone with PE does notice abnormal changes in their breathing, chest pains, rapid heart rate or other symptoms, they might assume it’s due to another less serious health problem. For example, such as a respiratory infection, acid reflux or passing illness.
What can you do to lower your risk for pulmonary embolism while you have the chance? Prevention and treatments for PE and DVT include: improving your diet, exercising, avoiding long periods of inactivity, and staying at a healthy weight. Use special precaution following injury to a vein, trauma, a hospital stay or post-surgery.
What Is a Pulmonary Embolism?
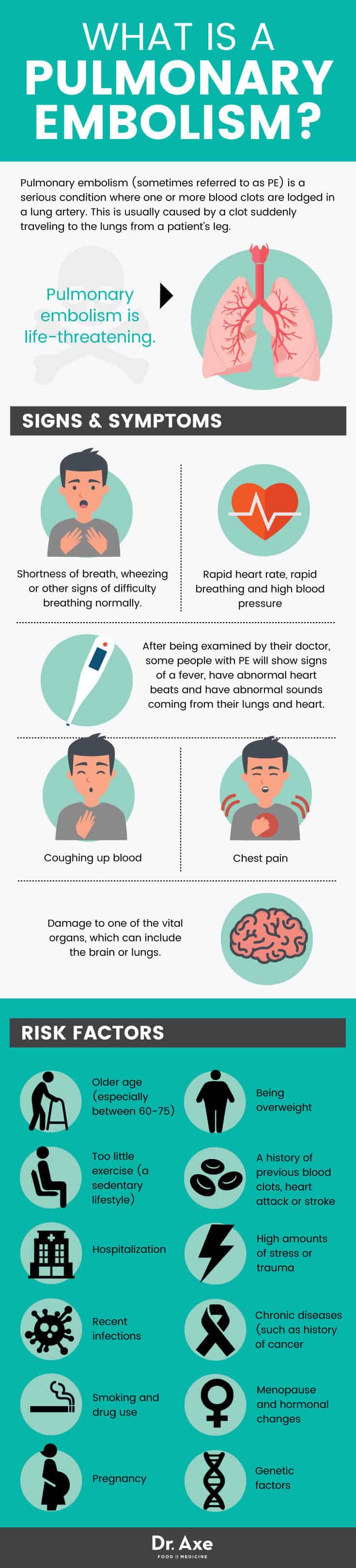
Pulmonary embolism (sometimes referred to as PE) is a serious condition. It’s characterized by having one or more blood clots in a lung artery. This is usually caused by a clot suddenly traveling to the lungs from a patient’s leg.
A blood clot in the leg is called deep vein thrombosis (or DVT). DVT sometimes results in the clot breaking away from its original location. Then the clot travels through the bloodstream to another part of the body, such as the brain or a lung. Once the clot blocks normal blood flow to one of the lungs, permanent damage due to reduced oxygen, or even death, can result. When left untreated, about 30 percent of patients who have PE will die due to tissue damage, death of healthy cells and complications.
Common Signs & Symptoms of Pulmonary Embolism
As stated above, symptoms don’t always occur due to pulmonary embolism. When symptoms do occur (often due low oxygen levels in the blood) they can include: (3)
- Shortness of breath, wheezing or other signs of difficulty breathing normally. Along with chest pains, having trouble breathing is the most common symptom of pulmonary embolism. Chest pains can sometimes feel similar to having a heart attack. They may occur during sleep or after a stressful episode. The National Institute of Health, called the Prospective Investigation of Pulmonary Embolism Diagnosis (PIOPED), conducted a large study. They found that 73 percent of patients with PE who had symptoms experienced some shortness of breath; 66 percent experienced chest pains; and 37 percent struggled with coughing. (4)
- Coughing up blood
- Rapid heart rate, rapid breathing and high blood pressure
- After being examined by their doctor, some people with PE will show signs of a fever, have abnormal heart beats and have abnormal sounds coming from their lungs and heart.
- Damage to one of the vital organs, which can include the brain or lungs. The term pulmonary hypertension refers to damage caused by increased pressure in the pulmonary arteries of the lungs. Pulmonary infraction is the condition caused by death of cells in the lungs, and damage to lung tissue because of a lower oxygen supply.
- Pulmonary embolism is life-threatening. When one or more clots travels to the lungs, or clots become big enough to seriously impair oxygen flow, death can occur. A very large embolism in the lungs can block the entire trunk of the pulmonary artery. It can cause lower blood flow to both sides of the lungs, and can lead to death almost immediately. This is why it’s critical to get help right away if you notice symptoms of DVT or PE.
Just like with pulmonary embolism, not everyone who has DVT will notice symptoms. Some signs that you might be at risk for deep vein thrombosis, which can lead to pulmonary embolism, include:
- Swelling and signs of inflammation in one of the legs where the clot has formed. This can include warmth, pain, tenderness and redness of the affected leg.
- Changes in skin appearance or color near the clot site. This might develop in only one leg or in both and spread up the legs from the clot location.
- Difficulty walking or moving normally.
- Sometimes scaling or ulcers form in the affected part of the body
- According to the National Heart, Lung, and Blood Institute, blood clots in the thighs are more likely to break off and cause complications than blood clots in the lower legs or other parts of the body.
Causes of Pulmonary Embolism and Risk Factors
Most blood clots (embolisms) that travel to the lungs are believed to come from deep veins of the lower body. The risk of developing serious complications and death depends mostly on the size of the blood clot that has traveled to the lungs. It also depends on the health of the patient’s veins. If a very large clot lodges inside the arteries near the lungs, blood cannot be pumped properly from the heart. This leads to death of healthy cells.
The PE patient’s health and age affects the seriousness of the problem. According to the Center for Disease Control & Prevention, people who are at the highest risk for death due to PE are those who already have partial blockages in their arteries, have experienced a recent vein injury, or who a history of heart disease. (5) People who are older and have many risk factors for pulmonary embolism, such as high levels of inflammation and arterial damage due to an unhealthy lifestyle, are much more likely to die from PE than younger, healthier people.
Risk factors for pulmonary embolism (which are similar to risk factors for deep vein thrombosis) include:
- Older age (especially between 60-75): The risk for blood clots increases with older age. Older adults are more likely to have arterial damage and risk factors for PE such as deep vein thrombosis compared to younger adults. This is especially true if they’re already suffering from another chronic illness, obese or overweight. The risk for PE in children is believed to be as low as 1 in 1 million. However, the risk doubles with each decade of life after the age of 40.
- Being overweight: Being very overweight or obese is linked to a higher risk for blood clots, due to changes in inflammation, blood pressure and possibly because of how excess fat tissue increases estrogen levels.
- Too little exercise (a sedentary lifestyle): An inactive lifestyle increases risk for poor blood flow and clot development. The highest risk is seen in those who have been very inactive due to factors like pregnancy, obesity, bed rest or surgery. These can all contribute to blood pooling. Although less of a risk, circumstances like taking long plane or car rides, sitting at a desk all day, watching TV for many hours and immobilization after surgery may lead to development of a clot that can start the process of DVT.
- A history of previous blood clots, heart attack or stroke: People who have a history of arterial damage, unhealthy blood pressure, a heart attack, stroke or heart disease are more likely to have clots than those without any history of cardiovascular problems. Those who have had injuries to veins, such from some surgical procedures or even traumatic impacts, can also develop an embolism or DVT more easily.
- Hospitalization: Around 20 percent of all cases of PE happen in the hospital. This is usually due to triggers like immobilization, healing from surgery, recovering from another illness, dealing with trauma or stress, blood pressure changes, being treated with an intravenous catheter (these increase risk for clotting) or infections.
- High amounts of stress or trauma: Experiencing a traumatic event (physical or even mental) may increase risk for DVT or PE tenfold! (06) Trauma and stress increase the level of clotting factors in the blood. They can also increase inflammation, change hormones and alter blood pressure levels.
- Recent infections: A recent serious infection increases risk for embolisms and DVT due to an effect on inflammatory processes, clotting and blood pressure.
- Chronic diseases (such as history of cancer, autoimmune disease or arthritis). Studies have found that a history of certain types of conditions including cancer, lupus, arthritis, diabetes, kidney disease and inflammatory bowel disease may all contribute to clots. Any condition that causes damage to blood vessels and cells in the lung may increase clotting.
- Smoking and drug use: All of the risk factors described above are worse when you smoke cigarettes, use other tobacco products, drink too much alcohol or use recreational drugs.
- Menopause and hormonal changes: Some research shows that changes in estrogen, including increased estrogen due to taking birth control pills or hormone replacement therapy drugs, can increase blood clotting and cause various heart complications. Menopausal women taking drugs to replace estrogen are also at a higher risk if they smoke, are overweight and don’t exercise.
- Pregnancy: Women seem to have a higher risk for developing clots during pregnancy and right after giving birth. Reasons for this include producing extra blood to support the fetus, more pressure being applied to veins, changes in blood pressure and obesity/weight gain. A scary finding is that pulmonary embolism is one of the leading causes of maternal death during birth.
- Genetic factors: Certain inherited traits can lead to genetic blood-clotting disorders, or the production of too many platelets. This causes blood to clot too easily and makes clot formation more likely. However, usually other risk factors are involved for a clot to form.
Related: How to Maintain Normal Troponin Levels
Conventional Treatments For Pulmonary Embolism & DVT
Pulmonary embolism is typically treated with a combination of blood-thinning medicines, procedures to remove clots, and prevention of future clots. The most important step in treatment is preventing an existing blood clot from getting bigger and keeping new clots from forming. Medications used to prevent clot formation by thinning the blood include: anticoagulants or blood thinners (either by pill, an injection, or through a needle or tube inserted into a vein), including Warfarin or Coumadin and Heparin.
Pregnant women usually receive Heparin only, as Warfarin is considered to be dangerous. These medications are typically prescribed for 3 to 6 months, but shouldn’t be used for much longer. While blood thinners can save lives, it’s also important to make lifestyle changes to help resolve the problem. Side effects from blood thinners are also possible. Plus, another clot can always come back if risk factors aren’t removed. The biggest problem associated with blood-thinners is bleeding. Bleeding can happen if too much medication is used and blood gets too thin. This side effect can be life threatening if an injury occurs that cannot be controlled.

5 Natural Remedies For Pulmonary Embolism
1. Improve Your Diet
Some people wonder if consuming foods with vitamin K (known to help with blood clotting) will increase PE risk. This doesn’t seem to be the case. In fact, foods like leafy greens that naturally provide vitamin K are very healthy options. They have many anti-inflammatory properties. Prioritize eating nutrient-dense, unprocessed foods, especially: leafy vegetables, non-starchy veggies like cruciferous veggies, avocado, sweet potatoes, olive oil, berries and bananas. These are high in crucial electrolytes, antioxidants and other nutrients. However, keep in mind that vitamin K can interact with blood-thinning drugs. Make sure you’re monitored if you’ve been prescribed these medicines.
Other foods, herbs and supplements that can have natural anticoagulant and anti-inflammatory effects to reduce risk for PE include: (07)
- Foods with vitamin E and vitamin D: found in fruits, veggies, cage-free eggs and certain types of mushrooms
- Spices and herbs, including garlic, turmeric, oregano, cayenne and ginger
- Real dark cocoa/chocolate
- Fruits such as papaya, berries and pineapple
- Raw honey
- Apple cider vinegar
- Green tea
- Fish oil and omega-3 fatty acids from wild caught fish
- Evening primrose oil
- Lean healthy sources of protein like beans, legumes, nuts, seeds, fish and pasture-raised meat in moderation
- Be sure to consume enough plain water and other hydrating liquids like herbal teas. Stay away from added sugar and too much alcohol or caffeine
2. Stay Active
Getting regular exercise and avoiding periods of prolonged inactivity, bed rest or immobilization can help lower your risk for PE. The best types of exercise for keeping your blood pressure at a healthy level, protecting your lungs and maintaining a strong heart and veins are aerobic exercises (like running, HIIT workouts or cycling) combined with resistance/strength-training. It’s highly important to maintain a regular exercise program into older age, as well as to make a strong point to move throughout the day more. Try to take breaks regularly from sitting and make sure to stretch. If you are at risk for PE, such as due to history of DVT, get up and move every 15 minutes during long car or plane trips and while sitting at work.
3. Maintain A Healthy Weight
Being overweight puts more pressure on your heart, vital organs, lower extremities and blood vessels. Estrogen stored in fatty tissue can contribute to clot formation, inflammation and other problems that can trigger development of a potentially dangerous clot. Keep a healthy weight even as you age by reducing intake of inflammatory, processed foods and eating a whole foods-based diet. Stay active, get enough sleep, watch your alcohol intake and reduce stress as well.
4. Check Your Medications
Medications including birth control pills, hormone replacement drugs (usually used by menopausal, postmenopausal women or those treating infertility) and medications prescribed to control blood pressure are all linked to higher incidence of blood clots, DVT and PE. Drugs used in cancer treatments or for managing autoimmune disorders may also interfere with blood clotting. (08)
Speak with your doctor about use of these medications if you have other risk factors for PE. You may need to lower or change your medications may if they might be contributing to any problems. Or, consider alternative ways to manage your health condition naturally. If you decide to take blood-thinning drugs (Coumadin or Jantoven, for example), your doctor will likely want to monitor you to make sure your dose is not too high or used for too long.
5. Take Precaution After Trauma, Injury, Surgery, When Traveling or When Hospitalized
Between 7-57 percent of people who experience some sort of traumatic injury wind up developing DVT or PE. Yet, venous thromboembolic events (VTE) after patients experience injury and hospitalization are highly preventable, according to a 2004 review published in the Annals of Surgery.
Ninety percent of patients who experience a dangerous event related to development of an embolism have at least 1 of the 9 risk factors commonly associated with DVT and PE. The six risk factors found to be most significant in predicting a major problem: being over the age of 40; suffering from a lower extremity fracture; suffering from a head injury; being on a ventilator for more than 3 days; recovering from venous injury; or having a major operative procedure. (09) Be sure to speak with your doctor if you have a history of any of these risk factors. Talk about your treatment options following surgery or trauma; research now suggests that certain medications and venous cava filters should be used only for patients who cannot receive any other form of care.
Related: Natural Blood Thinners You Already May Have in Your Kitchen
Precautions If You Suspect Pulmonary Embolism: When To Get Help Right Away
It can be hard to see PE coming, but this doesn’t mean you shouldn’t look out for signs and symptoms. If you experience shortness of breath or sudden chest pains— especially if you have multiple risk factors for an embolism, a history of DVT or a history of heart disease—see your doctor right away. Always seek emergency care if you have swelling suddenly in an arm or your leg (a sign of DVT) along with chest pains and breathing problems.
Be very mindful of any embolism symptoms that might develop, including: after surgery, after getting out of the hospital, when recovering from a serious illness or injury (especially if the injury affects the legs), after recent immobility such as bed rest, or when recovering from some type of serious trauma and stressor.
Final Thoughts On Diagnosing & Treating Pulmonary Embolism
- Pulmonary embolism (PE) happens when a blood clot forms (usually in one of the legs) breaks off, and then travels through the bloodstream to the lungs causing a blockage. This can be life-threatening and cause death in about 30 percent of patients.
- Risk factors for PE include: deep vein thrombosis, obesity, heart disease, a sedentary lifestyle, trauma and hospitalization.
- Ways to treat PE naturally include preventing blood clots from forming, eating a healthy diet, exercising, and maintaining a healthy weight.










