This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Lupus Symptoms to Keep an Eye On & What to Do About Them
May 31, 2016

You may have heard of lupus, but do you know the most common lupus symptoms to look out for? You should, because this autoimmune disease affects at least 1.5 million Americans and more than 5 million people worldwide. (1)
Even more alarming, more than 16,000 new cases of lupus are reported each year in the U.S. alone. This is especially serious for women, particularly those who are young to middle-aged women of childbearing age, because about 90 percent of lupus patients are women.
The good news is if you identify lupus symptoms early enough, you can prevent or naturally treat lupus. So, what is lupus exactly and what are the symptoms of lupus you need to be aware of? Read on to find out.
What Is Lupus?
Lupus is a type of chronic autoimmune disorder that affects many different organs in the body, causing symptoms that impact nearly every aspect of someone’s life. For example, rashes, mood changes, chronic fatigue, headaches and bodily pains are all common lupus symptoms. Lupus affects many more women than men, but both sexes and people of all ages and ethnicities can develop lupus. (2)
According to a report published in the Maedica Journal of Clinical Medicine, because lupus symptoms are similar to many other illnesses — including thyroid disorders, fibromyalgia, adrenal fatigue, Lyme disease and other autoimmune disorders — it can be hard for patients to receive a proper diagnosis of lupus. (3) Some experts have even nicknamed lupus “the great imitator” because lupus symptoms are often confused with various other health problems, often leading to a long road of recovery for patients. Most people with lupus are diagnosed in their 20s or 30s, sometimes after years of “not feeling right” and visiting many different practitioners for tests.
Lupus is an autoimmune disease because it’s a problem of the immune system. It’s caused by a combination of genetic and lifestyle factors. But having a family history is not a guarantee for developing lupus, nor is it contagious. Symptoms of lupus vary from mild to life-threatening, often coming and going based on other events in someone’s life.
Although it’s a chronic disease that poses serious risks, a lot of people with lupus can manage their disorder well with treatment and are able to carry on mostly normal lives. Today, lupus is treated with conventional medications — including immunosuppressant drugs and anti-inflammatory medications — but it can also be managed naturally with complementary treatments, such as herbs, chiropractic adjustments, massage therapy, meditation and a nutrient-dense diet.
Lupus Symptoms & Warning Signs
Lupus affects every person differently, and there are a wide range of symptoms that can be attributed to the disease. There are two kinds of lupus that cause different sets of lupus symptoms: discoid lupus erythematosus (DLE) and systemic lupus erythematosus (SLE). DLE mainly affects skin and is usually triggered by exposure to sunlight that causes skin lesions. But DLE usually doesn’t damage internal organs or glands. Systemic lupus, on the other hand, affects the entire body and is more serious. (4)
A third variation of this disease is known as drug-induced lupus (DILE). Functionally, drug-induced lupus operates similarly to SLE, damaging systems throughout the body. As you probably guessed, this particular form of lupus is a reaction to medication, usually taken consistently for a minimum of three to six months. Entire medication groups have been cited as the predicators, including anti-convulsants (for seizure prevention), beta blockers, sulfonamides and, as of 2016, proton pump inhibitors (PPIs) used to treat acid reflux symptoms. (5, 6)
Drug-induced lupus is generally reversible and symptoms often end within days or weeks of discontinuing the problematic medication. In rare cases, a patient might experience a kidney inflammation called nephritis that requires serious treatment. These infections are associated with drug-induced lupus caused by TNF-inhibitor drugs. (7)
Certain lupus symptoms are usually only temporary (like skin rashes on the face), while others can be persistent and cause serious complications (such as joint pain, blood clotting or ongoing fatigue). Lupus is considered a chronic autoimmune disorder because symptoms tend to last longer than six weeks and often for many years, unlike other autoimmune disorders that might go away more easily with lifestyle changes, such as Hashimoto’s disease.
Although lupus is much more common in women, lupus symptoms in women and men are usually the same. However, anyone with lupus who experiences high amounts of stress is more likely to experience worsened lupus symptoms due to having lower immune function. (8) The majority of people who suffer from lupus experience episodes, or “flares,” and remission.
Symptoms tend to become worse for a period of time but then go away afterward, only to come back at a later time. Because lupus symptoms are always coming and going, especially in response to stressful events, this is another reason lupus is difficult to recognize and diagnose.

According to the Lupus Foundation, the most common signs and symptoms of lupus include: (10)
-
- Extreme Fatigue: Approximately 90 percent of all people with lupus experience some level of fatigue and lethargy, according to the Johns Hopkins Lupus Center. (11) This can make it hard to work, exercise, take care of a family and keep up with everyday demands. Some find it helpful to take a 90-minute midday nap, although this is not possible for everyone. Your doctor may actually recommend that you try staying more active than usual to combat fatigue.
- Recurring Fever: Having recurring low-grade fevers around 99–101 degrees Fahrenheit is one of the earliest signs of lupus and could be a sign of inflammation or infection. While these do not reach the high temperatures usually accepted as severe fever (at least 101 degrees), these low-grade fevers often signal oncoming lupus flares, although they may also be indicative of infection or illness.
- Muscle/Joint Pain: Stiffness and swelling can occur around certain affected joints or muscles. Certain joints might also appear red, inflamed and warm, and pain might get worse when moving.
- Poor Circulation: Poor circulation in extremities is known as Raynaud’s phenomenon and causes fingers and toes to turn white or blue for a short period of time.
- Skin Rashes: This includes a rash on the face that covers the cheeks and bridge of the nose. Estimates show that about 50 percent of people with lupus experience a butterfly-shaped facial rash, hives and photosensitivity (sensitivity to sunlight). Redness, peeling and itchiness can sometimes develop. Some people also develop lesions on their skin about the size of a coin called discoid lesions.
- Photosensitivity: Many people with lupus easily become sun-burned, develop skin lesions and have skin itchiness caused by sun exposure.
- Respiratory and Heart Symptoms: Lupus symptoms can include pulmonary and respiratory problems, like easily becoming short of breath and having chest pain, since the lungs and airways can become inflamed due to swelling. Pleuritic chest pains (also referred to as pleurisy) are a symptom caused by inflammation of the diaphragm and swelling of the blood vessels around the lungs (pleuritis).
- Anemia: Many people with lupus develop anemia (a lack of either red blood cells or total blood volume). This contributes to fatigue and other problems.
- Fluid Retention/Swelling: Swelling (edema) is especially common in the feet, legs, hands and/or around eyes or face.
- Poor Fluid Production: Sjögren’s syndrome is sometimes triggered by lupus, which is a type of autoimmune disorder that affects the glands responsible for the production of tears and saliva. The eyes can feel gritty or dry due to lupus, and ulcers can also form inside the mouth or around the nose. Other people with lupus experience damaged blood vessels in their eyes and nerve damage that makes it hard to control movement of the eyes. Sjögren’s syndrome may also cause a dryness of the mouth and vagina.
- Digestive Problems: Lupus symptoms of the digestive tract can include loss of appetite, heartburn, acid indigestion or other gastrointestinal problems. GI problems tend to get worse with stress and sometimes cause a loss of appetite and weight loss. Weight loss can occur in patients with active SLE, but some who take corticosteroid medications to fight the disease might start to gain a lot of weight unintentionally.
- Insomnia: Many people have trouble sleeping normally, sometimes caused by sleeping too much during the daytime due to fatigue.
- Hair Loss: Due to scalp inflammation and irritation, hair can fall out by the clump or slowly, a condition known as alopecia. Facial or body hair might also fall out, including the eyebrows or eyelashes. Some people also experience brittle hair that breaks easily and won’t grow back.
- Loss of Libido: This can be due to stress, fatigue and hormonal changes. Lupus symptoms for women might also include vaginal dryness and irregular periods.
- Headaches: Having headaches can be a sign of a large number of issues, but it is a common lupus symptom.
- Ulcers: A patient with lupus might experience nose or mouth ulcers.
- Mood Changes: This includes cognitive impairments, such as brain fog, confusion and memory loss. In fact, a third of lupus patients are diagnosed with clinical depression.
Lupus Complications
Lupus is a serious illness and poses the risk for various complications if left untreated and unmanaged. Some complications associated with lupus can include:
- Lung Damage: A complication called vanishing (or shrinking) lung syndrome can develop when the diaphragmatic muscles become very weak and the lungs literally start to shrivel up and move. This causes shortness of breath and higher susceptibility to infections. It is thought that shrinking lung syndrome affects about one in every 200 people with SLE. (12)
- Kidney Damage: Nephritis is a type of kidney inflammation that develops when the kidneys cannot properly filter toxins and waste from the blood. This can cause swelling, high blood pressure, blood or dark colors in the urine, and pain above the kidneys. Usually with lupus nephritis is a complication associated only with drug-induced lupus as a result of TNF-inhibiting drugs.
- Metabolic and Thyroid Disorders: Lupus raises the risk for autoimmune thyroid diseases, which can negatively impact someone’s metabolism, menstrual cycle or hormone levels, weight, heart, skin, kidneys and liver. Symptoms can vary a lot since some people with lupus experience an underactive thyroid (hypothyroidism) while others have an overactive thyroid (hyperthyroidism). Estimates suggest about 6 percent of lupus patients suffer from underactive thyroid, while 1 percent generally have overactive thyroid issues.
- Connective Tissue and Nerve Damage (known as neuropathy): Lupus is capable of causing damage to the spinal cord and brain, which affects nerve signaling and also neurotransmitter production. This is one reason that people with lupus develop cognitive impairment, mood changes, and even seizures or stroke. Studies have found that people with lupus are also more likely to deal with the effects of anxiety and depression due to a complex combination of biochemical abnormalities that affect different parts of the brain.
- Increased Risk of Heart Disease: Long-term inflammation caused by lupus can damage the heart and blood vessels. It can also cause pericarditis, an inflammation of tissue surrounding the heart. The risk of heart disease for lupus patients seems to be somewhere between 8–16 percent of cases, while it is between 1.4–4.1 percent for the average person without heart disease risk factors. (13, 14, 15)
- Cutaneous Lupus Erythematosus: This is a complication of lupus involving the skin-related symptoms often presented with SLE. Cutaneous lupus affects at least 50 percent of SLE patients. It can occasionally occur without a person first developing another form of lupus, in which case the patient will be subsequently diagnosed with SLE in about 10 percent of cases. Cutaneous lupus has four classifications, depending on the way it develops and severity of symptoms: acute, subacute, intermittent and chronic.
- Neonatal Lupus: Not a “true” type of lupus, neonatal lupus occurs when a mother with lupus passes certain antibodies to her unborn child that cause minor cutaneous lupus symptoms, liver problems or low blood counts. This diagnosis is extremely rare, and even rarer is the possibility that the newborn might develop congenital heart block, which is often found by a doctor at 18–24 weeks gestation and can often be treated before or right after birth. Unfortunately, children who have a heart block can’t be entirely cured and will probably require a pacemaker at some point in their lives. Neonatal lupus affects very few children of lupus-afflicted mothers, while most children of moms with lupus don’t have the disease. (16)
Lupus Facts & Numbers
- The Lupus Foundation of America reports that at least 1.5 million Americans have lupus (and more than 5 million people throughout the world have it). This number might even be much higher, but it’s a hard disorder to diagnose and large studies/surveys reporting the prevalence rate have not been conducted.
- Every year in the U.S. alone more than 16,000 new cases of lupus are reported.
- Women are most likely to develop lupus, especially young to middle-aged women of “childbearing age” (between the ages of about 15–44). About 90 percent of all lupus patients are women. (17) Pregnancy, menopause and hormonal changes can all contribute to lupus. Lupus flares during pregnancy are not usually life threatening to the mother or fetus.
- Men, children, older women and teenagers can also develop lupus, especially if they’re African-American, Asian or Native American. People of these ethnicities are believed to be two to three times more likely to develop lupus than Caucasians.
Lupus vs. Lyme Disease: How Are They Related and Different?
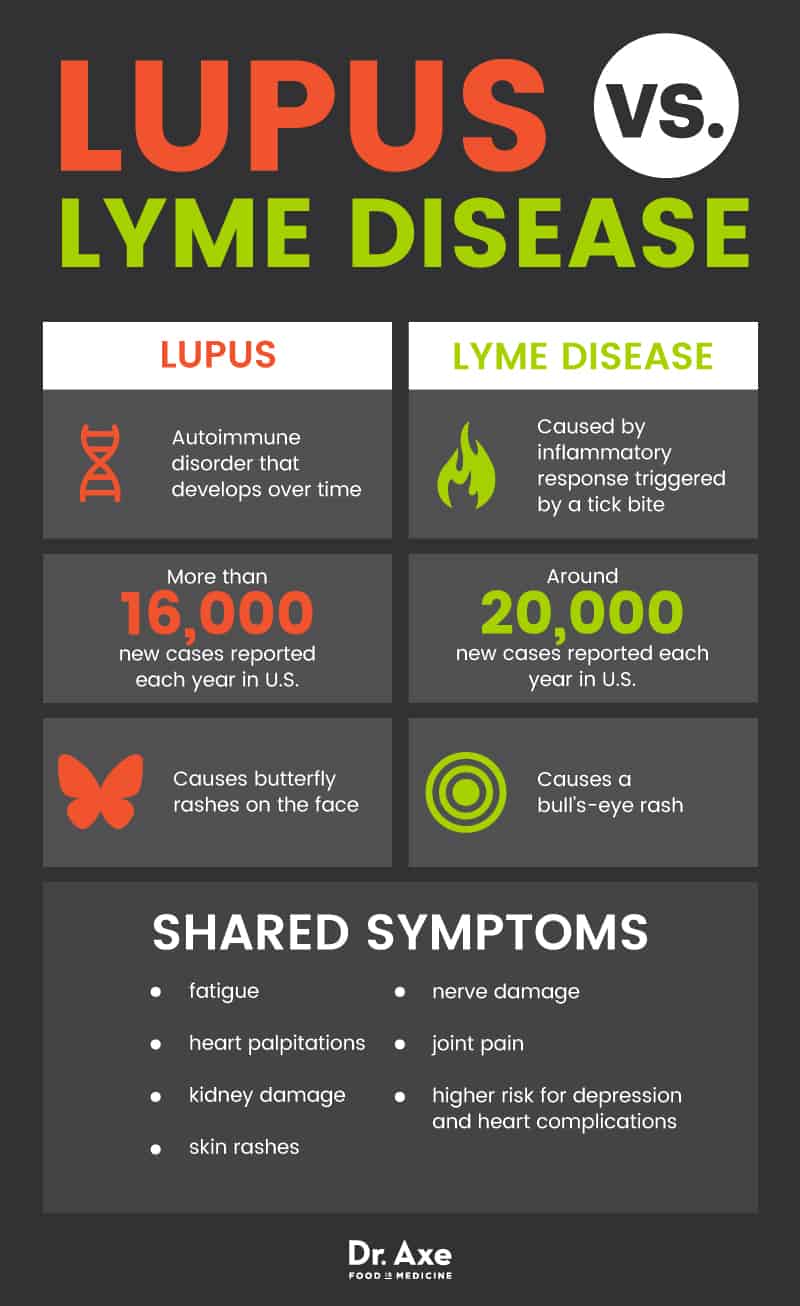
Many lupus symptoms are the same as Lyme disease symptoms — not to mention other common health problems caused by inflammation and autoimmune reactions like rheumatoid arthritis, blood disorders and diabetes.
Symptoms that Lyme disease and lupus have in common include:
- fatigue
- heart palpitations
- kidney damage
- skin rashes
- nerve damage
- joint pain
- higher risk for other problems like depression and heart complications
Doctors often confuse these two illnesses initially and are careful to track symptoms over time in order to be able to tell them apart, which is very important considering they have different causes and treatment approaches.
While lupus is an autoimmune disorder that can develop over time, Lyme disease is caused by an inflammatory response that’s triggered initially due to a tick bite. The exact way that Lyme disease progresses is controversial and still under a lot of debate. The Centers for Disease Control and Prevention (CDC) states that there are around 20,000 new cases of Lyme disease identified each year in the U.S. alone, especially during the summer when tick bites are more common.
Both Lyme disease and lupus cause skin rashes for many people, although the two usually appear differently on the skin. A “butterfly rash” on the face is most common with lupus, while a “bull’s-eye” rash (called erythema migrans) is more common with Lyme disease. (18) Kidney malfunction and damage is another shared symptom along with electrolyte imbalances, dizziness, weakness, changes in urine and dehydration.
One serious complication that can occur due to both disorders is atrioventricular block, which is caused by a dangerous blockage in heart vessels and sometimes reoccurring heart palpitations and blood pressure problems. In patients with lupus, atrioventricular block is normally triggered by electrolyte imbalances and kidney malfunctioning, while in Lyme disease patients it’s caused by inflammation of the heart.
Atrioventricular block (also called AV block) results in inflammation of the atria and ventricles of the heart, changing the way nerve impulses travel to and from the heart (similar to atrial fibrillation). Sometimes atrioventricular block goes away on its own, but other times it can lead to permanent damage that triggers other heart problems and requires a pacemaker or other interventions to control. (19)
As you’ll learn below, just like with lupus, managing Lyme disease naturally involves boosting immune function, lowering bacterial infections, and treating toxicity, gut problems and inflammation.
6 Natural Treatments for Lupus Symptoms
1. Preventing Nutrient Deficiencies
Nutrient deficiencies lower immune function, can contribute to fatigue, and make you more susceptible to illnesses like viruses and infections. People with lupus should make it a priority to eat a well-rounded, unprocessed diet in order to maintain a healthy body weight, keep blood pressure levels within a healthy range, control cholesterol and prevent fatigue.
A healthy lupus diet includes:
- fresh vegetables and fruit
- sources of omega-3 fats like wild-caught salmon
- nuts and seeds
- coconut oil
- bone broth
- lean sources of protein
In fact, a 2016 study on mice found that consuming DHA (docosahexaenoic acid), an omega-3 fatty acid, stopped lupus symptoms triggered by crystalline silica. According to Jack Harkema, a researcher in the study, “Ninety-six percent of the lung lesions were stopped with DHA after being triggered by the silica.” (20) You can get DHA from consuming wild-caught salmon, sardines, herring and mackerel or by taking an omega-3 fish oil supplement. (21)
One specific food that people with lupus should avoid is alfalfa seeds and alfalfa sprouts, since certain compounds in alfalfa have been shown to trigger the immune system. It seems likely that the amino acid L-canavanine may further activate the immune system, causing inflammation and prompt a lupus flare. (22)
2. Getting Enough Rest, Relaxation and Sleep
High amounts of stress can weaken the immune system and cause hormonal changes that lead to inflammation. Stress also makes fatigue worse and interferes with sleep. Managing stress and getting enough sleep are very important for controlling lupus symptoms because lupus patients are already at a heightened risk for depression, anxiety, confusion and memory loss. (23)
Sleeping for at least eight to nine hours daily and reducing stress through meditation, healing prayer, therapy, exercise, yoga or tai chi, creative projects and time spent outdoors can also help manage lupus symptoms.
3. Avoiding Smoking and Toxicity Exposure
Smoking increases lung damage and also raises the risks for lupus complications like heart disease, stroke and infections. Cigarettes can also impair immunity, slow down blood flow, raise blood pressure levels and worsen skin inflammation. Similarly to other autoimmune conditions, lupus is linked to smoking. One way to cut down on your risk of developing this disease or having constant flares is to quit smoking immediately. (24)
Other chemical toxins that contribute to lupus and worsen inflammation include trichloroethylene (found in unfiltered water and sometimes dust), endocrine disruptors, and chemicals from household or beauty products, such as paints, hair products and dyes.
4. Staying Active
Exercise is important for people with lupus because it helps keep joints flexible, makes the heart and lungs stronger, helps raise immune function and control stress, as well as helps manage weight, which can also be an issue for lupus patients. (25) Since many people with lupus experience muscle and joint pains on top of intense fatigue, low-impact activities like walking, cycling, swimming, yoga, dancing, water aerobics and Pilates are all good choices for activities.
5. Protecting Your Skin
Lupus can be triggered by sun exposure and also causes skin to become extra fragile and vulnerable to burns and sun damage. Make sure to protect your skin from sunburns by staying out of the sun during the brightest hours of the day, using nontoxic sunscreen with a sun protection factor of 50 or higher, wearing sunglasses, and wearing a hat. Natural products should also be used on the skin that won’t worsen inflammation and irritation, instead of beauty products with synthetic ingredients and chemicals. (26)
6. Increase Your Vitamin D Intake
Recently, researchers have discovered an interesting connection between vitamin D deficiency and lupus. While the evidence does not suggest that a deficiency of vitamin D actually causes lupus, it is likely the two are connected. Studies have found that 67 percent or more of lupus patients do not have enough vitamin D in their bloodstream. (27) You may want to try adding a high-quality vitamin D supplement to your regimen.
What Causes Lupus?
Although the exact cause of lupus isn’t known, experts know that lupus is triggered by abnormal changes in someone’s immune system. Like other autoimmune disorders, the immune systems of people with lupus are mistakenly triggered into fighting healthy tissue and cells within the body because of the false impression that the body is being threatened. (28)
The immune system produces a certain type of antibody that reacts with “self-molecules” (molecules that are a natural part of the body) called autoantibodies. In a healthy human body, these autoantibodies are tolerated by normal cells but activated when the body recognizes foreign cells and designed to attack the unknown cells. (29)
Autoantibody activation is considered a sign of autoimmune condition onset, like that of lupus. For an unknown reason, autoantibodies start to recognize normal human cells as dangerous foreign invaders, attacking the cells and causing tissue damage and system malfunctions throughout the body. This takes place through what is known as the classical complement pathway. (30, 31)
Some of the glands, organs and tissues damaged by lupus include the thyroid gland, heart, gut/digestive system, lungs and kidneys. The immune system can produce numerous autoantibodies that contribute to lupus, especially one type called antinuclear antibodies.
Genetics play a role in the development of lupus, and experts think that certain people are born with genes that impact the way their immune systems work, making them more susceptible to getting lupus. Other risk factors for lupus include: (32)
- taking certain medicines that affect the immune system
- toxicity and exposure to chemicals
- poor gut health and leaky gut syndrome
- nutrient deficiences
- allergies
- smoking cigarettes
- a history of infections
- high levels of stress that wear down the immune system
- hormonal imbalances, such as estrogen dominance
- pregnancy
- overexposure to UV light (usually sunlight)
Is it lupus or psoriatic arthritis?
A condition commonly confused with lupus is psoriatic arthritis. This form of arthritis is usually preceded by the development of psoriasis, although it’s not unheard of for people to develop arthritic symptoms as a result of psoriasis before ever noticing the skin lesions associated with the condition. (33)
The tests for psoriatic arthritis often include X-rays, while lupus is generally diagnosed by a doctor observing symptoms over time since no single test exists to determine a lupus diagnosis.
Both conditions often display rashes and swelling/stiffness of the joints. However, a lupus rash is usually butterfly-shaped and covers the nose and cheeks, while psoriasis lesions occur in various places on the body and can look a number of different ways.
Your doctor should be able to determine which, if either, condition you may have.
Lupus and Cancer
The connection between lupus and cancer is a complex one. Lupus is not a form of cancer, but having lupus seems to increase or decrease the risk of certain cancers for unknown reasons.
For example, your risk of lymphoma, lung, bladder, liver, kidney and thyroid cancers seems to be somewhat elevated with lupus. (34, 35) Suggested reasons for this are often pinpointed as the immunosuppressive drugs conventionally used to treat the disease, which increase the risk of specific cancers such as lymphomas and blood cancers, particularly after five or more years of consistent use. When it comes to lung cancer, most lupus and lung cancer sufferers are smokers, which is why it’s especially important not to smoke if you have lupus.
Most sources agree that breast and ovarian cancer risk actually goes down with the development of lupus, although no one has been able to pinpoint why these hormonal cancers would occur less often in these patients. (36, 37)
The two hormonal cancers that are something of a mystery include prostate cancer in men and cervical cancer in women. There are conflicting findings about the correlation between lupus and these cancers. More often, it seems these two cancers
seem to occur less often in people with lupus. (38) However, some reports have found an increased risk for both cervical and prostate cancer in lupus patients. (39)
One report at an American Urological Association annual meeting, though not peer-reviewed, found prostate cancer to occur five times more often in men diagnosed with SLE and 10 times more often in those with DLE. Unlike some of the reviews that found the opposite correlation, the subject pool of this one was massive — they examined data on 189, 290 men with autoimmune diseases (not all of which were lupus). (40)
Even with these reports, it’s important to realize that the best way to protect yourself from cancer (and all disease) is to manage your diet by eating whole, life-giving foods and avoiding foods that cause inflammation and oxidative stress, limiting your exposure to harmful chemicals and sustaining an active lifestyle.
In addition, do your best to find out what causes any irregular symptoms you have that could point to cancer, such as having regular prostate exams or breast exams after the age of 40 and visiting your doctor to determine the cause of irregularities in your body.
Lupus Key Points
- Lupus symptoms can vary, including fatigue, swelling, joint pain, headaches, nerve damage and skin rashes.
- Lupus is an autoimmmune disease that doesn’t have one single cause but is triggered by a combination of factors, including genetic inheritance, inflammation, a poor diet, poor gut health, toxicity and stressful life episodes.
- Natural treatments for lupus include eating an anti-inflammatory diet, resolving nutrient deficiencies and allergies, controlling stress, exercising, and protecting the skin from too much sun exposure.
- It is possible to live a full life, even after a lupus diagnosis. Research finds that the disease is non-fatal in most cases — in fact, 90 percent of people with lupus live normal lifespans. (41) By managing your diet, toxin exposure, stress load and following the advice of a physician you trust, you should be able to live a long and healthy life.
6 Natural Treatments for Lupus Symptoms
- Eat a well-rounded, unprocessed diet.
- Get enough rest and stress relief.
- Avoid smoking and exposure to toxins.
- Stay active.
- Protect your skin from sunburn.
- Increase your vitamin D intake.








