This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Cellulitis Symptoms, Causes & Risk Factors
December 14, 2016
The name of the bacteria responsible for most cases of cellulitis infections and cellulitis symptoms is staphylococcus, which is actually very common and lives on the skin of approximately 30 percent of even healthy adults. Cellulitis skin rash is one of the most common symptoms of a staph infection, which cause all kinds of mild to moderate symptoms ranging from skin blisters all the way to serious, life-threatening heart complications.
Estimates show that around 5 percent of people staying in American hospitals will develop some type of staph infection due to their stays, usually in the form of a skin infection. Proper hygiene and disinfection in hospitals can cut back on the amount of infections patients develop by around 40 percent. (1) Although antibiotics are normally capable of controlling cellulitis symptoms and stopping the infection from spreading further, increasingly they’re not always a reliable treatment option. A growing number of cases of cellulitis infections are now antibiotic-resistant, meaning the bacteria causing the infection (MRSA) continue to reproduce despite multiple courses of medications.
When is comes to protecting yourself from cellulitis, preventing the infection from developing in the first place is key. Ways to lower your risk include increasing immunity with a healthy diet, avoiding toxins or drugs that can weaken your immune system, and keeping your skin clean by practicing good hygiene.
What Is Cellulitis?
The official cellulitis definition is “an acute infection of the dermal and subcutaneous layers of the skin.” In other words, cellulitis is a bacterial infection that affects the skin, sometimes spreading quickly as bacteria penetrate deeper to tissues below the skin. (2)
The bacteria that cause cellulitis usually enter the skin through open cuts or wounds, then reproduce rapidly once making their way into small, enclosed pockets within certain tissue. The infection caused by these bacteria triggers cellulitis symptoms like skin redness, pain and tenderness, along with the formation of painful blisters. Some also develop large, inflamed abscesses below the skin’s surface or symptoms of a fever, such as chills and weakness.
Cellulitis symptoms develop due to the body’s inflammatory responses (the body trying to protect itself from fighting the bacteria), as well as from irritation and swelling caused by the growth of bacteria.
The bacteria responsible for cellulitis cause cellulitis symptoms directly because they produce metabolites and enzymes that aggravate/irritate the tissues of the skin. Because symptoms get worse with time as bacteria have the chance to keep proliferating, prompt attention and treatment of the infection is very important to prevent permanent damage or spreading.
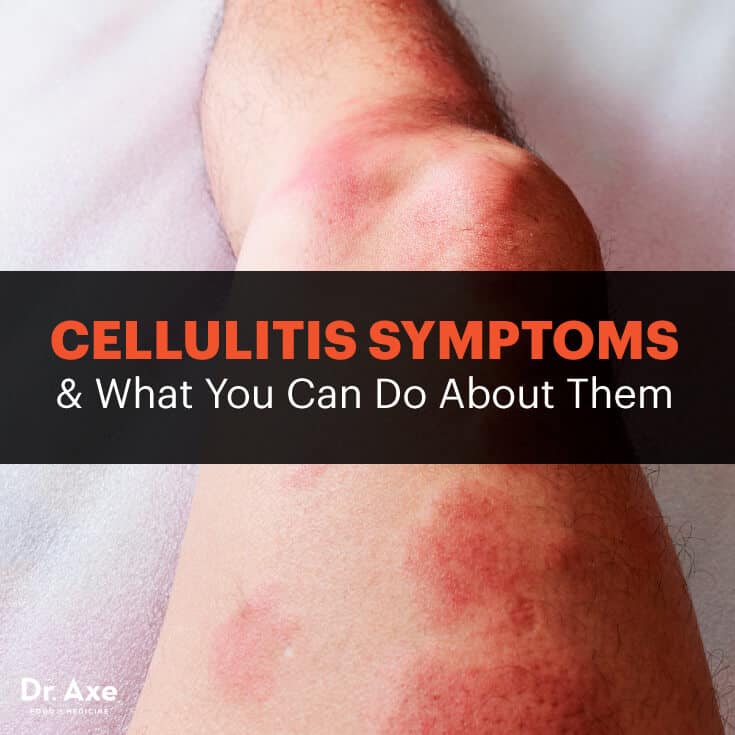
Cellulitis Symptoms
Cellulitis affects the skin and other layers of tissue just below the surface of the skin. Sometimes the bacteria that cause cellulitis infections can also spread into the bloodstream and then to vital organs, such as the heart or lungs, although this isn’t commonly the case. Normally only one side of the body is affected by cellulitis infection, such as one hand or one leg — unlike other illnesses that usually cause skin symptoms to develop on both sides of the body (like allergies or psoriasis). Parts of body that develop cellulitis symptoms most often are:
- the legs
- the hands
- anywhere on the skin that has an open wound, incision or wound
The reason these areas of the skin become infected with cellulitis most often is because they tend to have the most open cuts/wounds, plus they easily hold excess fluid inside (called edema) and accumulate pus. This causes swelling and the formation of abscesses, or pockets in the skin where bacteria can hide out and keep repopulating.
According to the Centers for Disease Control and Prevention (CDC), the most common cellulitis symptoms are: (3)
- Redness of the skin, which becomes worse as the skin rash due to infection spreads
- Pain on the surface of the skin or pain when pressing the infected area. Pain and redness are usually the first symptoms to emerge and indications that treatment is needed.
- Tenderness over certain swollen areas of the skin, especially when skin becomes very inflamed and hot
- Changes in the color of skin, including turning orange or bright red
- Developing pus or fluid-filled blisters. Small blisters on the skin are called vesicles, while large ones are called bullae. Sometimes blisters might appear yellow, and a center/head may form where pus accumulates.
- Symptoms of a fever, including fatigue, weakness, chills and sometimes nausea/vomiting. Some also experience rapid heart rate, headaches, low blood pressure, dizziness and confusion.
- Sometimes the infection causes swelling in the lymph nodes (called lymphadenitis) or inflammation of the blood vessels in the lymphatic system (called lymphangitis)
Cellulitis Causes
Cellulitis is a bacterial infection, meaning it’s triggered from certain harmful microbes entering the body and causing an inflammatory response. There are a number of different bacteria that can cause cellulitis, with the two most common being Streptococcus and Staphylococcus. (4)
Streptococci bacteria are capable of reproducing and spreading very quickly, so they contribute to other infections as well. These bacteria produce enzymes that aggravate the skin and stop the immune system from preventing the bacteria from proliferating.
Staphylococcus bacteria are more likely to cause infections by entering the skin through open wounds. Once they make their way deeper into the tissue below the surface of the skin, they tend to repopulate within small pockets — causing the accumulation of pus, increased swelling, and sometimes the formation of abscesses that are filled with dead cells and fluid.
More recently other types of bacteria that have become resistant to antibiotics have also started causing cellulitis infections. This is a very dangerous condition because these infections are very difficult to treat. A type of Staphylococcus bacteria strain called methicillin-resistant Staphylococcus aureus (or MRSA for short) has been found to be capable of surviving even with use of previously effective antibiotic treatments. MRSA is now a growing concern globally and increasingly causing life-threatening symptoms that can affect the entire body.
More serious cellulitis systemic infections have also been found to be due in part to presence of strains like Vibrio vulnificus or Streptococcus pneumoniae. (5)
Risk Factors for Developing Cellulitis Symptoms and Infections
The biggest risk factor for developing cellulitis infections is having any exposed cuts, wounds or scrapes on the skin — even small ones. These can be due to experiencing injuries that cause bleeding/scabbing, recovering from fractures, post-surgery after an incision has been made, from burns to the skin, or following fungal infections.
Examples of some skin conditions that can contribute to cellulitis infection symptoms include athlete’s foot, eczema, shingles or chicken pox, and skin disorders that cause picking at the skin or bleeding (such as cystic acne). These cause cracks to form in the surface of the skin that allow more bacteria to enter and proliferate — however they usually aren’t the sole reason for infection. (6)
Another important factor contributing to infection is having a weakened immune system. Most people already have the bacteria that causes cellulitis on their skin, however they don’t develop infections because they’re able to control how much the bacteria continue to reproduce. Several conditions that can weaken someone’s immune system and raise the risk for many different viruses and bacterial infections include autoimmune disorders, such as lupus, diabetes, leukemia and HIV/AIDS. Being very stressed, obese, taking corticosteroid medications, smoking cigarettes and using drugs can also negatively affect the immune system.
“Antibacterial overkill” and poor gut health are also risk factors since the frequent use of antibacterial products and medications can prevent our immune systems from learning how to defend us against invaders. This makes our immune systems highly reactive throughout our adult years (a concept known as the hygiene hypothesis), making it harder to prevent bacterial infections (including cellulitis or staph infections) from developing. Poor gut health also raises the risk for other health problems tied to lack of “good bacteria” in our bodies, such as allergies, hay fever, autoimmune disorder symptoms and asthma, for example.
Cellulitis vs. Lyme Disease: They’re Often Confused, So How Do They Differ?
It’s possible for Lyme disease symptoms that affect the skin (including a red rash) to be confused with other infections, including cellulitis, dermatitis or gout.
Lyme disease can cause a rash that looks like a red ring around a swollen area expanding outward (erythema with central clearing). However, many patients also develop a rash that looks more like cellulitis without the appearance of a central ring (homogenous erythema).
In patients with lifestyles that put them in a high-risk category for Lyme disease, the CDC recommends that an accurate diagnosis be made using reputable tests that are carried out through a laboratory with experience in testing for Lyme disease. (7) A combination of visiting a dermatologists familiar with cellulitis and/or consulting with emergency or internal medicine departments seems to be the best way to differentiate these two conditions.
Since the standard Elisa screening test for Lyme misses at least 35 percent of cases, it’s also best to obtain assistance from a Lyme-literate doctor when any questions come up regarding whether symptoms might be due to another illness. Doctors belonging to the International Lyme and Associated Diseases Society look at tests and investigate your symptoms to make a clinical diagnosis.
In some cases, it’s possible for patients to become infected with both, since a weakened immune system is tied to both. Evidence suggests that co-infected patients tend to have more symptoms, more severe symptoms and have symptoms for a longer duration compared to patients with only one infection.
Conventional Treatment for Cellulitis Symptoms
In most cases when a patient develops cellulitis, antibiotics are prescribed right away to treat the infection. While antibiotics don’t always work to resolve cellulitis symptoms (such as in the case of MRSA infections that are resistant to antibiotics), research shows that usually antibiotics do help stop the infection from spreading and reaching the bloodstream or internal organs.
Antibiotics used to treat cellulitis include the types called dicloxacillin, cephalexin, trimethoprim with sulfamethoxazole, clindamycin or doxycycline. These are normally taken for five to 10 days or sometimes up to 14 days if the infection continues to cause symptoms. Doctors usually prescribe drugs that are effective against both streptococci and staphylococci bacteria, however remember that sometimes the infection can become resistant to antibiotics.
People who have already developed serious infection symptoms by the time they seek help are normally hospitalized and given antibiotics intravenously in order to reduce the infection as quickly as possible. Treatments given by vein for severe cellulitis infections include oxacillin or nafcillin. When complications don’t develop due to cellulitis, in most cases symptoms usually go away within several days following these treatments. Some patients actually experience worsened symptoms before they start to get better. When large amounts of cellulitis bacteria die, they can leave behind irritating byproducts that can cause the skin to keep reacting by raising inflammation. If this is the case, it can take more than one week (around seven to 10 days) for cellulitis symptoms to subside.
Natural Treatments for Cellulitis Symptoms and Infection
Prevention and natural treatments for cellulitis include boosting immunity with a healthy diet, avoiding antibacterial overkill as described above, cleaning and protecting any open cuts on the skin, washing your hands regularly, and treating skin pain with heat and essential oils. Some of the most reliable ways to help prevent and treat cellulitis naturally are:
1. Draining Skin Abscesses to Decrease Swelling/Pain
Other than using antibiotics, doctors may choose to open and drain an infected cellulitis abscess below the surface of the skin to relieve fluid or pus buildup and lower swelling. Drainage is used most often when the infection is very severe, such as when it causes cellulitis symptom complications like:
-
Large violaceous bullae (fluid-filled sacs below the skin that cannot drain)
-
Hemorrhage below the skin
-
Skin sloughing or numbing/anesthesia
-
Rapid spreading
-
Gas forming in the tissue
-
Blood pressure changes
When edema, blisters or abscess formations become very bad, the patient is normally kept immobile in the hospital (such as putting the patient on bed rest), cool and damp to help the skin heal and reduce internal swelling/heat. The body part where the infection develops is also elevated, while wet dressings or bandages might be applied along with ointment.
2. Practice Good Hygiene to Prevent Future Infections
Keeping the skin clean and improving circulation (blood flow) to the skin are important for preventing infections. Here are several steps to practice good skin hygiene:
- Wash and moisturize the skin using natural products, especially if you have any cuts or after being near anyone who is sick.
- Inspect cuts or wounds for signs of infection. Keep cuts covered with a bandage, and apply ointment to help healing.
- Wear clean clothes and undergarments.
- Treat fungal infections quickly.
- Wash your hands before touching open cuts in your skin.
- Don’t share items like razors or other products that touch the skin.
3. Treat Pain with Natural Skin Care Products
To help ease discomfort caused by the infection, including blisters and inflammation, some of the following methods can be used:
- Press a warm compress against the rash once or twice daily using a fresh, clean washcloth or towel.
- Soak inflamed skin under a warm shower (but not too hot) or in a warm bath.
- Very gently stretch stiff areas to keep them from getting even more stiff.
- Wear loose, breathable clothing made from natural fibers.
- Keep any chemical products or skin irritants off the affected area (perfume, scented body soaps, detergents, lotions, etc.).
- With clearance from your doctor first, apply natural antibacterial essential oils, such as lavender, to the skin, combined with a moisturizing carrier oil, such as coconut oil, several times daily.
Cellulitis Facts and Figures
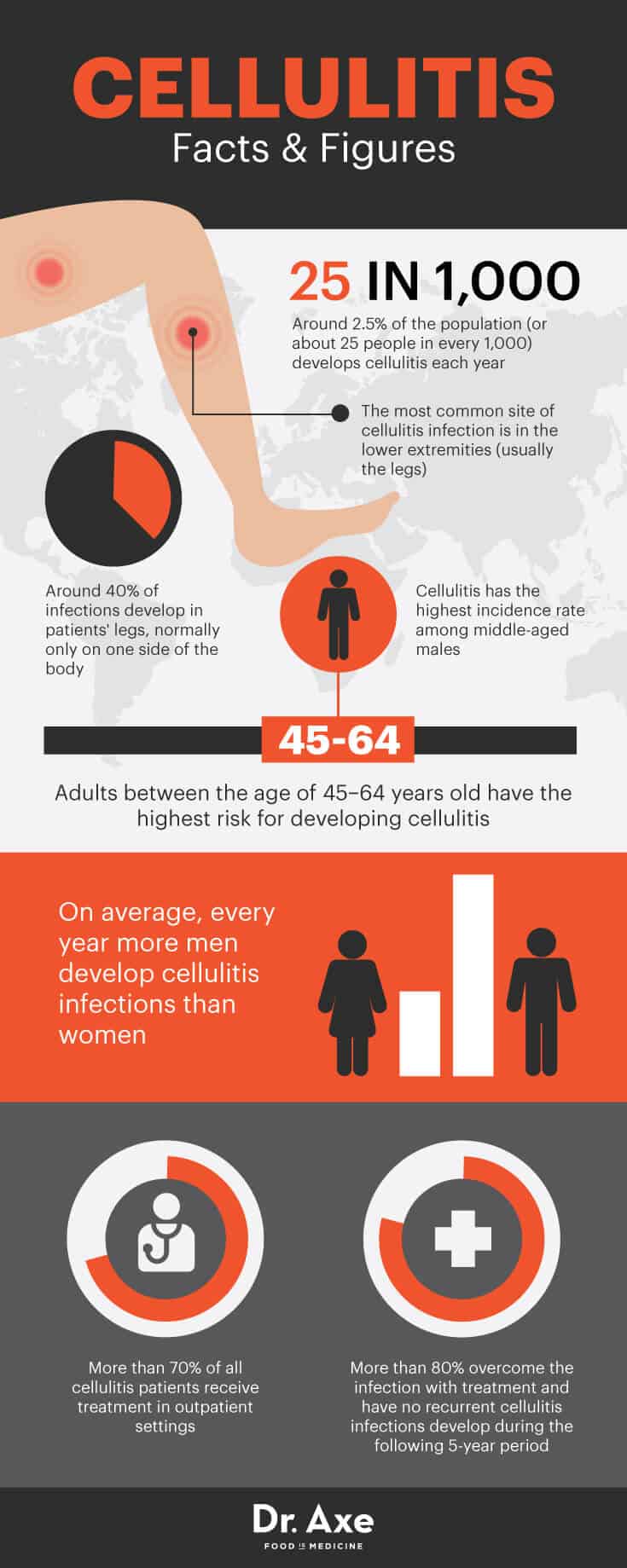
- Around 2.5 percent of the population (or about 25 people in every 1000) develops cellulitis each year.
- Cellulitis has the highest incidence rate among middle-aged males. On average, every year more men develop cellulitis infections than women.
- Adults between the age of 45–64 have the highest risk for developing cellulitis. (9)
- The most common site of cellulitis infection is in the lower extremities (usually the legs). Around 40 percent of infections develop in patients’ legs, normally only on one side of the body.
- More than 70 percent of all cellulitis patients receive treatment in an outpatient setting. More than 80 percent overcome the infection with treatment and have no recurrent cellulitis infections develop during the following five-year period.
Precautions Regarding Cellulitis Symptoms
If you experience any of the cellulitis symptoms described above, always visit your doctor for an evaluation and guidance regarding treatment, since the infection can sometimes be very serious. It’s also possible to develop some of the symptoms associated with cellulitis (like redness and tenderness in one leg or hand) but actually be suffering from another condition altogether — such as deep vein thrombosis, which causes similar symptoms.
While cellulitis symptoms can usually be managed well with treatment, especially when caught early, sometimes complications are possible. While rare, complications due to cellulitis can include the development of large abscesses that keep coming back in the same part of the body, damage to the lymphatic vessels, permanent swelling of the affected tissue, permanently destroyed skin tissue and the spreading of bacteria through the blood (called bacteremia, which is life-threatening).
Anyone who is seriously ill before developing cellulitis symptoms, who has a weakened immune system due to another medical condition, who is recovering from surgery or who is elderly should take cellulitis very seriously. The CDC recommends that blood culture tests be taken in patients who are in the following circumstances:
- Have any moderate to severe disease affecting the skin
- Have cellulitis returning after previously being treated
- A history of contact with potentially contaminated water
- Recovering from any animal bite that caused puncturing of the skin
- Patients receiving chemotherapy
- Pregnant women
- Those with cell-mediated immunodeficiency
Final Thoughts on Cellulitis Symptoms
- Cellulitis is a bacterial infection that affects the skin, sometimes spreading deeper to tissues below the skin. In serious cases, the bacteria that cause cellulitis infections can also spread into the bloodstream and then to vital organs, such as the heart or lungs, causing complications.
- Symptoms of cellulitis include skin redness and pain, tenderness and heat/swelling over the affected area, skin blisters or abscesses, and sometimes symptoms of a fever.
- Risk factors for developing cellulitis include have a weakened immune system, poor gut health, having open cuts or wounds on the skin, and not practicing good hygiene.
