This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Adenomyosis: Enlarged Uterus Causes (+ 6 Tips for Pain Relief)
January 24, 2018

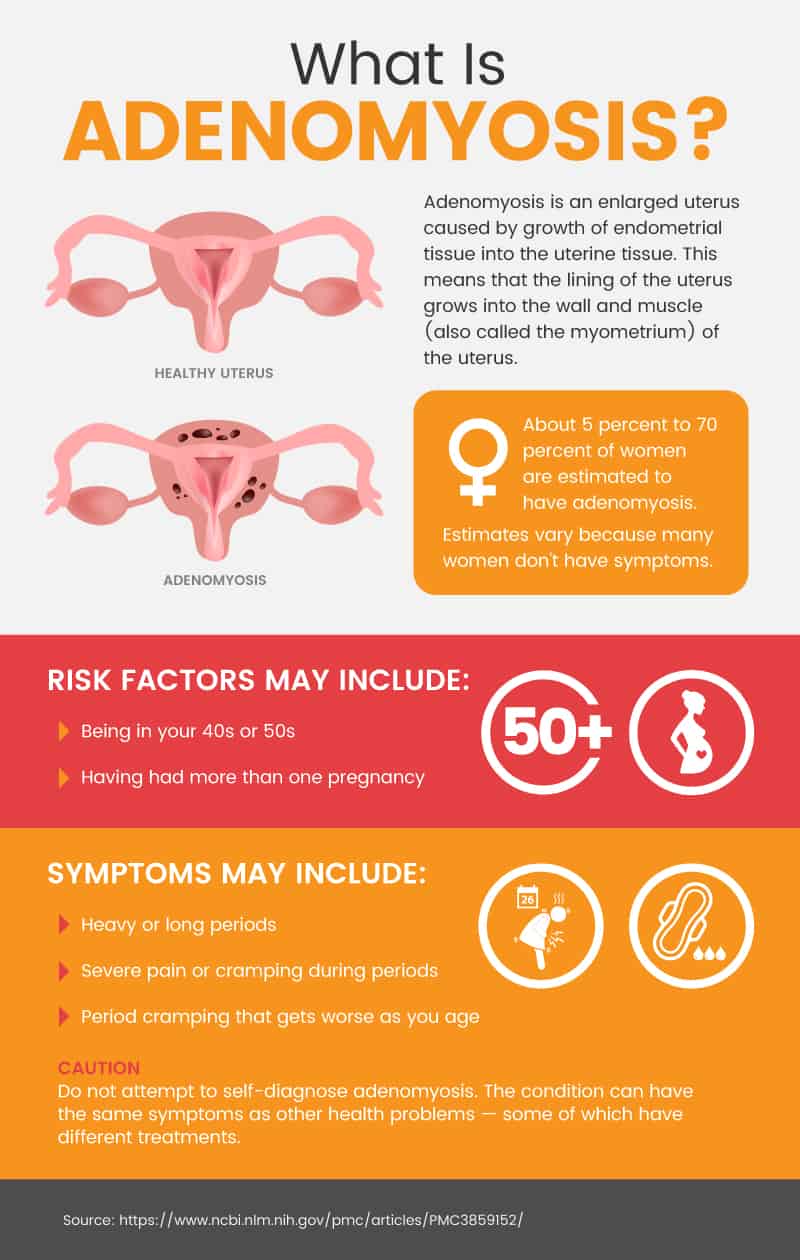
Adenomysosis affects many women, usually in their 40s and 50s. It is an enlargement or thickening of the uterus. It happens when the uterus lining, called endometrial tissue, starts growing inside the actual wall and tissue of the uterus. (1)
Although adenomyosis can cause painful, heavy periods for some women, it often does not cause any symptoms at all. Thankfully, those who do experience adenomyosis symptoms can get full relief once they enter menopause or get a hysterectomy. There are also natural and conventional ways to manage symptoms for this fairly common but underdiagnosed condition.
What Is Adenomyosis?
Adenomyosis is an enlarged uterus caused by growth of endometrial tissue into the uterine tissue. This means that the lining of the uterus grows into the wall and muscle (also called the myometrium) of the uterus. The tissue keeps working just like the uterine lining — it gets thicker and then breaks down every month during your period. (2)
It is not clear how common adenomyosis is since many women do not have symptoms. Estimates range from 5 percent to 70 percent, but 8 percent to 30 percent is probably a more accurate range. (3) It is most common in women in their 40s and 50s who have had children. (4)
Adenomyosis depends on estrogen circulating in a woman’s body. When the estrogen levels go down (for example, at menopause or after a hysterectomy), adenomyosis symptoms stop. (5)
Adenomyosis vs. endometriosis
Adenomyosis is when endometrial cells are present in the uterus. Endometriosis is when endometrial cells grow in places outside of the uterus, such as the pelvis or lower abdomen. (6, 7) The two can have very similar symptoms, and sometimes doctors won’t know the difference until they do a surgery to find out if the cells are growing where they shouldn’t be or until they remove tissue or the uterus (called a hysterectomy).
Is it dangerous to have an enlarged uterus?
In general, adenomyosis is not dangerous. In women with severe symptoms, however, heavy menstrual bleeding can lead to anemia, which causes fatigue. The excessive bleeding and pain can also lead women to avoid activities and socializing, which can strain relationships and lead to depression, anxiety and other emotional distress. (8)
Is adenomyosis a cancer?
No, adenomyosis is not a type of cancer. However, adenomysois can result in a mass or lump of tissue called an adenomyoma. (9) These are basically benign (non-cancerous) tumors. They may look like uterine fibroids. Some people worry that adenomyosis and cancer of the endometrium or uterus may go hand in hand, but there doesn’t appear to be an increased risk of cancer among women with adenomyosis. (10, 11) Of course, some people with the condition will also have cancer, but it’s not believed that adenomyosis increases the risk. (12)
Can adenomyosis cause infertility?
In severe cases, adenomyosis that causes adenomyomas can lead to infertility in young women. (13) It is possible that adenomyosis itself can also cause infertility or trouble conceiving, but more research is needed. (14)
Possible problems conceiving may be due to the changes the disease can cause in the lining of the uterus or because it commonly co-occurs with endometriosis. (15) Adenomyosis and pregnancy are not necessarily incompatible, however. Many women with adenomyosis can conceive either naturally or with artificial assistance. (16) Normally, however, adenomyosis is diagnosed in women late in their childbearing years or after women have had children.
Adenomyosis Signs & Symptoms
In some cases, adenomyosis causes no symptoms at all. However, other women may experience the following adenomyosis symptoms: (17, 18)
- Heavy or long periods
- Severe pain or cramping during periods
- Period cramping that gets worse as you age
- Passing blood clots during periods
- Spotting between periods
- Pain in the pelvis or belly
- Pain during sex
Can an enlarged uterus cause constipation?
In short, yes. General symptoms of an enlarged uterus, which can be caused by fibroids and other conditions as well, may include: (19)
- Bloating
- Constipation
- Unexplained weight gain or a swollen lower belly
- Frequent urination
- Pain
- Fertility problems
Causes & Risk Factors
Causes of adenomyosis
Adenomyosis causes are mostly unknown. (20) However, there are several theories about possible adenomyosis causes: (21)
- The endometrial tissue invades the uterus
- The tissue was there from the time your body was formed as a fetus
- Inflammation from childbirth disrupts the boundary between the endometrium and uterine wall
- Bone marrow stem cells enter the uterine tissue and cause new growth of endometrial tissue
What causes the uterus to be enlarged?
In the case of adenomyosis, uterus enlargement is caused by endometrial cells growing throughout the normal uterine tissue. Endometrial tissue thickens naturally as part of its growth and shedding process. The uterus may also become inflamed, or swollen, from the misplaced endometrial tissue, which can also increase its size. Finally, it is common for women with adenomyosis to have other growths in the uterine wall that can increase the size of the uterus.
Risk factors for adenomyosis
Risk factors may include: (22)
- Being in your 40s or 50s
- Having had more than one pregnancy
- Previous surgery on the uterus, including C-sections and some types of abortions
- Use of tamoxifen for breast cancer
Conventional Treatment
Most women with adenomyosis do not require treatment. The condition is hard to diagnose and many times can only be confirmed after a hysterectomy. For women who are close to menopause, treatment may be less aggressive than for younger women unless symptoms are severe. This is because adenomyosis usually disappears after menopause, when estrogen levels drop. (23)
For women with adenomyosis symptoms, conventional treatment may include: (24, 25, 26, 27)
- Over-the-counter (OTC) anti-inflammatory drugs such as ibuprofen.
- Hormonal birth control. Pills that have a combination of estrogen and progestin or patches or rings that have this combination are sometimes prescribed to relieve pain and bleeding. Progestin-only pills or intrauterine devices can also cause periods to stop, which also stops period-related symptoms.
- Tissue destruction. Procedures such as endometrial ablation and MRI-guided focused ultrasound surgery try to destroy the endometrial tissue that is causing adenomyosis. These procedures may not work for everyone and more research is needed.
- Hysterectomy. This is surgical removal of the uterus. It permanently cures adenomyosis but is a major surgery. Adenomyosis hysterectomy is only done for women who have severe symptoms and who do not wish to have any more children.
Adenomyosis: 6 Natural Tips to Manage Symptoms
Natural treatments for adenomyosis generally involve managing the menstrual pain and bleeding caused by the condition.
Natural tips for managing adenomyosis symptoms include:
- Use heating pads
- Get massage therapy or acupressure
- Try herbs and supplements
- Alter your diet
- Exercise
- Ask about TENS
-
Use heating pads
In a review of studies looking at drug-free ways to relieve menstrual pain, heat (from heating pads, hot water bottles, etc.) was found to be effective in some cases. (28) Another study examined the use of a heat patch placed on the lower abdomen during menstruation and found that it was effective in making pain less severe. (29)
-
Get massage therapy or acupressure
- Massage with essential oils: In a study comparing the use of lotion with essential oils to lotion with synthetic fragrance, women with painful periods were told to massage their lower abdomens with the cream every day from the end of one period to the beginning of the next. The group with the essential oil-based cream had fewer days of pain during the next period. (30) The oils used (diluted in the cream!) were lavender, clary sage and marjoram. The oils contain pain-relieving compounds that the study authors suspect caused the reduction in menstrual pain.
- Another study using just lavender oil found that it was more effective than regular exercise at providing pain relief for women with painful periods and that after three cycles it was also effective at reducing anxiety. (31)
- Massage with aromatherapy: Another study found that women with painful periods who massaged their abdomens with rose oil experienced more pain relief than women who used unscented almond oil or no oil at all. (32) Women were told to massage their abdomens on the first day of two periods in a row, but the significant pain-relieving effects didn’t kick in until the second cycle.
- Acupressure: In a study that compared women with painful periods who received acupressure to women who did not receive it, the group who received acupressure had less severe pain immediately after and for the next two hours. (33)
-
Try herbs and supplements
A wide variety of herbal remedies have been used throughout history and around the world for painful, long or heavy periods. Some options with research supporting their usefulness for pain relief, mood improvement, or bleeding reduction include:
- Valerian: A high-quality study found that valerian was effective at reducing pain during a period when given in 255 milligram doses three times per day for three days at the start of a period, for two periods in a row. (34) The researchers believe the herb worked because of its antispasmodic effects.
- Rosa damascena (Damask rose): A study compared the use of a painkiller to Rosa damascena extract on painful periods. The two worked equally well and were effective in reducing pain intensity. (35)
- Chinese herbal medicine: Some research suggests that combinations of Chinese herbs may help with painful periods. (36) The most popular (based on prescriptions in Taiwan) are Corydalis yanhusuo, Cyperus rotundus, and Dang-Gui-Shao-Yao-San, or combinations containing these herbs. (37)
- Rhubarb (Rheum emodi): Women taking capsules of rhubarb powder twice a day for two days before their period started and throughout the first three days of their period had a significant decrease in pain and its duration. (38) In this study, other symptoms and quality of life were also better after taking the capsules to treat their period-related pain.
- Vitamin B1 and vitamin E: In a review of human studies, vitamin B1 at 100 milligrams per day was identified as an effective pain relief option for painful periods. A review of trials using herbal and dietary supplements to treat period-related symptoms found positive effects for women who had painful periods taking vitamin B1 and vitamin E. (39)
- Frankincense and myrrh: In a study in mice with painful periods (measured by signs of pain such as writhing), myrrh water extract, frankincense extract and a combination of the two were effective at reducing inflammation and pain. (40) Although the doses in the study are not scaled for humans, the anti-inflammatory and pain-relief abilities of these herbs may also help women with painful periods.
- Magnesium: In a review of studies of natural pain relief for painful periods, magnesium was effective at reducing pain. However, the studies used different doses so there is no clear dose that is known to be the best option. (41)
- Omega-3 fatty acids: In a small trial comparing fish oil to placebo pills, fish oil was more effective at relieving menstrual pain. (42)
- Chamomile: In a large review of natural therapies for menstrual pain, one study was identified that found chamomile to be more effective than OTC non-steroidal anti-inflammatory drugs (NSAIDs). (43)
Other possible herbs and supplements with some support in terms of formal research include fenugreek, fennel, ginger, chasteberry, cumin, a combination of fish oil and vitamin B1, peppermint, “true” cinnamon or Cinnamomum zeylanicum, thiamine, pyridoxine, zataria, and zinc sulphate. (44, 45, 46)
In general, however, there is virtually no data on safety. (47) If you choose to use herbal remedies or supplements for menstrual pain or heavy bleeding, do so with caution. Consult a health care professional before you start any new herbs or supplements, since they can interact with other medications.
-
Alter your diet
There is little specific research on diet and adenomyosis. However, many studies have investigated the relationship between diet and menstrual pain.
- Include omega-3 fatty acids: Endometriosis is more common in women with a lot of trans-fatty acids in their diet, and it is less likely in women who eat a lot of long-chain omega-3 fatty acids. (48) Since fish oil has also been found to reduce menstrual pain, it may make sense to eat a diet rich in omega-3 fatty acids and low in trans fats. (49, 50) Healthy sources of omega-3 fatty acids include fish such as mackerel and salmon, walnuts, chia seeds, flaxseeds, hemp seeds and egg yolks.
- Eat low-fat dairy: Abdominal bloating and pain during your period may be less likely if you eat three or four servings of dairy per day. (51)
- Consider a low-fat vegetarian diet: In a review of dietary and other treatments for painful and heavy periods, a low-fat vegetarian diet was identified as a possibly helpful way to reduce symptoms. (52)
- Eat lots of fiber: Women who ate a diet high in fiber had significantly less menstrual pain than women who didn’t in a Japanese study looking at multiple diets. (53)
According to the University of Maryland Medical Center, other dietary changes you can make to reduce period-related pain include: (54)
- Eat foods rich in calcium and antioxidants.
- Avoid processed or refined foods, such as white bread.
- Get your protein from lean meat, tofu or beans.
- Avoid caffeine and alcohol.
- Don’t smoke.
- Stay hydrated, drinking about six to eight glasses of water every day.
-
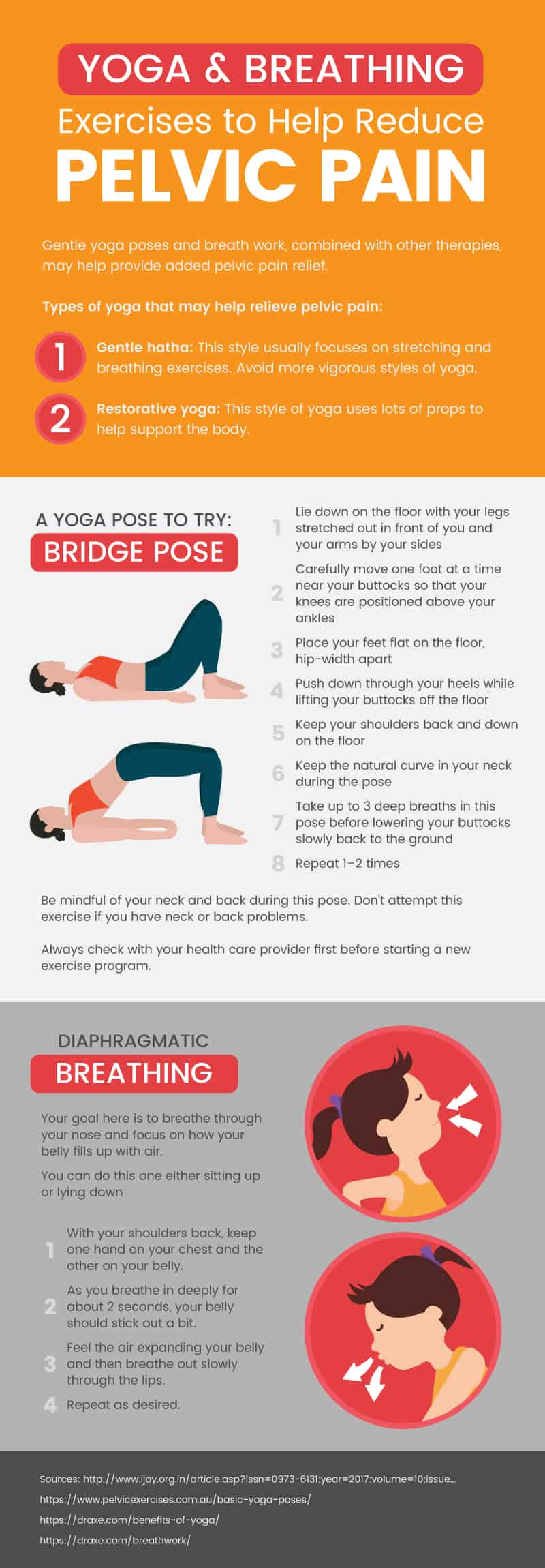
Exercise
A healthy body mass index is important for avoiding certain dysfunctions that can cause heavy periods. (55) For this reason, physicians often recommend regular exercise. Exercise can also limit anemia and improve energy and quality of life. (56) A review of several exercise studies found that exercise reduced pain and distress related to periods and stayed effective over time (rather than only helping for the first cycle). (57) In another review of studies on painful periods, exercise emerged as a possible way to improve blood flow to the pelvis, stimulate the release of endorphins, and thereby relieve pain. (58)
Despite general support for the importance of exercise, there are others who say that the jury is out. However, these researchers still acknowledge the probability that regular exercise is helpful for painful periods and is certainly helpful for other health conditions that are also important to women’s health. (59)
-
Ask about TENS
Transcutaneous electrical nerve stimulation (TENS) uses electric current to provide pain relief. By placing little electrodes on the skin, different frequencies of current enter the skin. In a study of TENS versus placebo, there was some evidence that TENS could give pain relief for patients with painful periods. (60) However, more research is needed. Ask a health care provider about whether TENS would be a safe and reasonable option for you if it interests you.
Precautions
Do not attempt to self-diagnose adenomyosis. The condition can have the same symptoms as other health problems — some of which have different treatments. Although you can manage many symptoms related to painful, heavy, or long periods at home, it is important to seek the care of a health professional if your period worries you or keeps you from doing activities you enjoy.
In addition, always consult a health care professional before taking new medications, herbs or supplements.
Adenomyosis Key Points
- Adenomyosis is very difficult to diagnose and is caused by the presence of endometrial tissue in the wall or muscle of the uterus.
- The condition often affects women late in their childbearing years and disappears once menopause begins.
- Most women with adenomyosis do not have symptoms or do not require treatment. However, some women have severe pain, heavy bleeding and other disruptive symptoms during their periods that get worse over time.
- Conventional management of adenomyosis typically includes over-the-counter pain relievers and anti-inflammatory drugs. In severe cases, women may receive surgery to destroy the endometrial tissue or to remove the uterus entirely.
Natural tips for managing adenomyosis symptoms at home include:
- Use heating pads.
- Get massage therapy or acupressure.
- Try herbs and supplements.
- Alter your diet.
- Exercise.
- Ask about TENS.








